Introduction:
Hepatitis A is a contagious liver infection caused by the hepatitis A virus (HAV). It’s a significant global health concern, particularly areas with poor sanitation and limited access to clean water. Here, we will explore the essential aspects of hepatitis A, including its causes, symptoms, diagnosis, treatment, and, most importantly, prevention.
Causes :
It is typically transmitted through the ingestion of contaminated food or water. Here are the primary causes and modes of transmission :
-
Fecal-Oral Route :
It is most commonly spread through the fecal-oral route. This means that the virus is present in the feces of an infected person and can be transmitted to others when they ingest food, water, or objects contaminated with the virus. The key factors contributing to this transmission include:
a. Contaminated Food
Consuming food that has been prepared by an infected person who did not follow proper hand hygiene and sanitation practices can lead to the ingestion of the virus.
b. Contaminated Water
Drinking water that is contaminated with the virus, which is particularly common in areas with poor sanitation and inadequate access to clean water.
c. Poor Hygiene
Inadequate handwashing after using the restroom or changing diapers, especially in public places, can contribute to the spread of the virus.
d. Close Personal Contact
Although less common, the virus can also be transmitted through close personal contact, particularly in households, by sharing personal items, or through sexual contact.
-
Travel to Endemic Regions :
People who travel to regions with high rates of hepatitis A are at an increased risk of contracting the virus, especially if they do not receive the hepatitis A vaccine or practice proper hygiene measures while abroad.
-
Consumption of Raw or Undercooked Shellfish:
In some cases, shellfish harvested from contaminated waters can carry the hepatitis A virus, posing a risk to consumers who eat them raw or undercooked.
-
Exposure to Infected Individuals :
Coming into contact with individuals who have hepatitis A and being exposed to their bodily fluids or personal items can result in transmission.
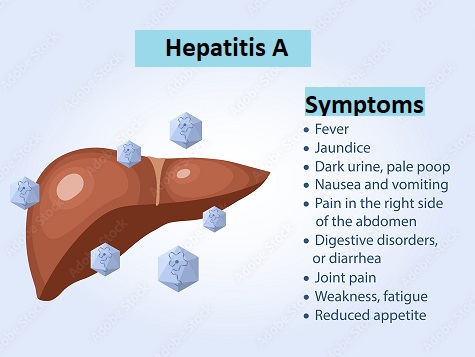
Symptoms of hepatitis A :
The symptoms can vary in severity and typically develop within a few weeks after exposure to the virus. Common symptoms include:
- Flu-Like Symptoms: Hepatitis A often begins with flu-like symptoms, which may include:
- Fever
- Fatigue
- Muscle aches
- Jaundice: Jaundice is one of the hallmark signs of hepatitis A. It is characterized by the yellowish discoloration of the skin and the whites of the eyes. This occurs due to the buildup of bilirubin, a yellow pigment, in the blood, as the liver’s ability to process it is impaired.
- Abdominal Pain: Many individuals experience discomfort and tenderness in the upper right side of the abdomen. This is due to the inflammation of the liver.
- Dark Urine: Urine may become darker in color, similar to the color of tea or cola. This change is also attributed to the accumulation of bilirubin.
- Pale Stools: Stools can become pale or clay-colored, which is a result of insufficient bilirubin reaching the intestines.
- Loss of Appetite: Hepatitis can lead to a significant decrease in appetite. Many people with the infection lose interest in eating.
- Nausea and Vomiting: Nausea is a common symptom, often accompanied by occasional vomiting.
- Itchy Skin: Some individuals may experience itching, known as pruritus, due to the effects of jaundice on the skin.
- Joint Pain: Joint pain, or arthralgia, can also occur in some cases.
- Fatigue: Hepatitis A often results in extreme tiredness and general weakness.
It’s important to note that not everyone infected with hepatitis A will experience all of these symptoms, and the severity of symptoms can vary. In some cases, particularly in children, it can be asymptomatic, meaning there are no noticeable symptoms.
How To Diagnosis :
The diagnosis of hepatitis A typically involves a combination of medical history, physical examination, and laboratory tests.
Here is an overview of the diagnostic process :
- Medical History and Physical Examination:
- The healthcare provider will start by taking a detailed medical history, including any recent travel, exposure to contaminated food or water, and known risk factors for hepatitis A.
- A physical examination may reveal symptoms and signs, such as jaundice (yellowing of the skin and eyes), abdominal pain, and an enlarged liver.
- Blood Tests:
- Blood tests are crucial in diagnosis. The following tests are commonly used: a. Hepatitis A Antibody Testing: This test measures the presence of antibodies against the hepatitis A virus. Two main types of antibodies are checked:
- IgM Antibodies: The presence of IgM antibodies indicates an acute or recent hepatitis A infection.
- IgG Antibodies: The presence of IgG antibodies suggests a past infection or vaccination. If IgG antibodies are detected, it means the individual has immunity to hepatitis A. b. Liver Function Tests: These blood tests assess the levels of liver enzymes and other markers to evaluate the overall function of the liver. Elevations in certain liver enzymes, such as alanine aminotransferase (ALT) and aspartate aminotransferase (AST), can indicate liver inflammation and damage. c. Bilirubin Levels: Elevated bilirubin levels, especially direct bilirubin, are associated with jaundice and liver dysfunction. d. Complete Blood Count (CBC): A CBC can reveal changes in the number of white blood cells, which may be elevated in response to infection.
- Blood tests are crucial in diagnosis. The following tests are commonly used: a. Hepatitis A Antibody Testing: This test measures the presence of antibodies against the hepatitis A virus. Two main types of antibodies are checked:
- Imaging Studies (in some cases):
- In severe cases or when complications are suspected, imaging studies like abdominal ultrasound or CT scans may be performed to assess the liver’s condition and rule out other potential causes of liver damage.
- Liver Biopsy (rarely):
- A liver biopsy is seldom required in diagnosis. It involves the removal of a small tissue sample from the liver for detailed examination. This invasive procedure is typically reserved for cases with atypical features or complications.
- Differential Diagnosis:
- The healthcare provider may also consider other potential causes of hepatitis-like symptoms, such as other viral hepatitis infections (hepatitis B or C), alcoholic hepatitis, or drug-induced liver injury. Differential diagnosis helps ensure the correct identification of the underlying cause.
Management :
The treatment of hepatitis A primarily focuses on managing the symptoms, providing supportive care, and allowing the body to recover naturally. Unlike hepatitis B and C, hepatitis A does not lead to chronic infection, and it usually resolves on its own without specific antiviral medications. Here are the key components of the treatment and care :
- Rest and Adequate Hydration:
- One of the most important aspects of managing hepatitis A is getting plenty of rest to allow the body to heal. Fatigue is a common symptom of the infection, and rest helps combat this.
- Staying well-hydrated is crucial, especially if you experience nausea, vomiting, or diarrhea. Drinking clear fluids, such as water or clear broths, can help prevent dehydration.
- Nutritious Diet:
- Maintaining a balanced and nutritious diet is important to support overall health and liver function. Even if you have a reduced appetite, try to eat small, frequent meals.
- Avoid alcohol and foods that are difficult for the liver to process, such as fatty or greasy foods.
- Medication Management:
- Avoid taking medications or supplements that can harm the liver. In particular, acetaminophen (paracetamol) should be avoided, as it can cause further liver damage when the liver is already compromised.
- Monitoring and Follow-Up:
- Regular medical check-ups are essential for monitoring the progress and ensuring that the infection is resolving as expected.
- Healthcare providers will closely monitor liver function through blood tests, including liver enzyme levels.
- Preventing Transmission:
- To prevent the spread of hepatitis A to others, it’s important to practice good hygiene, including thorough handwashing after using the restroom and before handling food.
- Individuals should avoid preparing or handling food for others until they are no longer contagious.
- Vaccination and Post-Exposure Prophylaxis:
- Hepatitis A vaccination can be administered to individuals at risk or those traveling to endemic regions to prevent infection.
- In some cases, a hepatitis A vaccine or immunoglobulin shot can be given as post-exposure prophylaxis to individuals who have been in close contact with a confirmed hepatitis A case, provided it is administered within two weeks of exposure.
It’s important to note that the majority of individuals recover fully within a few weeks to a few months without any long-term liver damage. However, in rare cases, hepatitis A can lead to severe liver complications. If you experience severe symptoms, such as persistent vomiting, severe abdominal pain, or confusion, or if your symptoms worsen, seek medical attention promptly.
Preventions :
Preventing hepatitis A is essential to reduce the risk of infection, especially since hepatitis A can cause discomfort and, in some cases, lead to severe illness.
Here are key strategies in prevention:
- Hepatitis A Vaccination:
- Hepatitis A vaccines are highly effective in preventing the disease. Both inactivated vaccines (given as injections) and a combination vaccine (hepatitis A and hepatitis B) are available.
- Routine vaccination is recommended for children, and it is also advisable for adults in specific risk groups:
- Travel to high hepatitis A prevalence area.
- Men who have sex with men.
- Individuals with chronic liver disease.
- People who use illegal drugs.
- Those in close contact with hepatitis A infected individuals.
- Workers in healthcare and food service settings.
- Some international travelers may also require vaccination based on their destination.

- Good Hygiene Practices:
- Proper handwashing is one of the most effective ways . Individuals should:
- Wash hands thoroughly with soap and clean, running water for at least 20 seconds, especially after using the restroom and before handling or consuming food.
- Encourage children to practice good hand hygiene.
- Avoid touching the face, mouth, or eyes with unwashed hands.
- Proper handwashing is one of the most effective ways . Individuals should:
- Safe Food and Water:
- Be cautious about the sources of food and water, especially when traveling to regions with inadequate sanitation.
- Avoid consuming raw or undercooked shellfish, particularly in areas with known hepatitis A risks.
- Ensure proper food handling and preparation practices at home and in restaurants.
- Safe Sex Practices:
- Practicing safe sex by using condoms can reduce the risk of sexual transmission of hepatitis A, especially among men who have sex with men.
- Post-Exposure Prophylaxis (PEP):
- If you’ve had close contact with someone diagnosed with hepatitis A, especially in the household or through sexual contact, consider receiving a hepatitis A vaccine or immune globulin (IG) shot for post-exposure prophylaxis. This should be received within two weeks of exposure.
- Travel Precautions:
- If you are traveling to areas with high prevalence, particularly in developing regions, consult with a healthcare provider about vaccination and follow safe food and water practices while abroad.
- Stay Informed:
- Being aware of hepatitis A risks in your region and staying informed about local outbreaks can help you take appropriate precautions.
Conclusion :
Hepatitis A is a preventable liver infection that can lead to severe illness and even death in some cases. By understanding the causes, recognizing the symptoms, and taking appropriate preventive measures, we can reduce the incidence of this disease and protect our health. Vaccination, good hygiene, and safe food and water practices play a critical role in combating hepatitis A and ensuring a healthier future for all.
Frequently Asked Questions (FAQ) About Hepatitis A :
What is hepatitis A?
It is a contagious liver disease caused by the hepatitis A virus (HAV). It can result in inflammation of the liver and is typically transmitted through contaminated food, water, or close personal contact.
What is the difference between hepatitis A and hepatitis B and C?
Hepatitis A is distinct from hepatitis B and C in several ways. It does not lead to chronic infection, and the body can usually clear the virus on its own. Hepatitis B and C, on the other hand, can result in chronic infections and long-term liver damage.
What is the most common early symptom of hepatitis A?
Typical symptoms include flu-like symptoms, jaundice (yellowing of the skin and eyes), abdominal pain, dark urine, pale stools, loss of appetite, nausea, vomiting, fatigue, and joint pain.
How is the disease diagnosed?
Diagnosis involves blood tests to detect antibodies to the hepatitis A virus, liver function tests, and sometimes imaging studies like ultrasound. A medical history and physical examination are also essential.
How do you control hepatitis A?
There is no specific antiviral treatment . The main focus is on supportive care, rest, hydration, and monitoring. Severe cases may require hospitalization.
Is it preventable?
Yes, it is preventable. Vaccination is highly effective and recommended, especially for individuals at risk or traveling to endemic areas. Good hygiene, safe food and water practices, and post-exposure prophylaxis are additional preventive measures.
Why everyone should get vaccinated?
The hepatitis A vaccine is recommended for children as part of routine childhood immunization. It is also advisable for adults in specific risk groups, such as travelers to high-risk regions, individuals with chronic liver disease, and healthcare and food service workers.
How can contamination from hepatitis A be prevented?
Practice good hygiene, especially thorough handwashing with soap and water. Avoid handling food for others and inform close contacts to seek post-exposure prophylaxis if they've been exposed.
Is hepatitis A considered an STD?
Yes, it can be transmitted through sexual contact, particularly among men who have sex with men. Using condoms can reduce the risk of transmission.
How long is someone with hepatitis A contagious?
People are mostly contagious for two weeks before and one week after the onset of symptoms. Proper hand hygiene and prevention measures are essential to reduce the risk of transmission.
Is there a cure for hepatitis A?
It is typically resolves on its own without the need for specific antiviral treatment. The focus is on managing symptoms and preventing complications.
Can you get hepatitis A more than once?
Generally, once you've had hepatitis A, you develop immunity against future infections. This means you are unlikely to be re infected .
Can you travel if you have hepatitis A?
Travel should be postponed until you are no longer contagious. Consult with a healthcare provider for guidance on when it is safe to travel after a hepatitis A diagnosis.