Fatty liver disease, medically known as hepatic steatosis, is a condition characterized by an excessive accumulation of fat in the liver cells. This condition can be benign or can progress to more serious liver damage. It’s becoming increasingly common worldwide, largely due to lifestyle factors such as poor diet and lack of exercise. This blog will explore the causes, symptoms, diagnosis, treatment, and prevention of fatty liver disease.
What is Fatty Liver Disease?
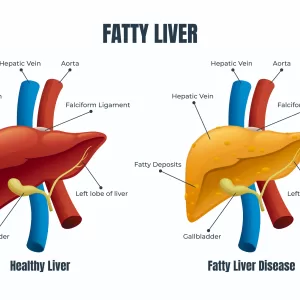
Fatty liver disease occurs when more than 5-10% of the liver’s weight is fat. This excessive fat can cause inflammation, damage liver cells, and interfere with normal liver function.
Types of Fatty Liver Disease
Fatty liver disease, characterized by an accumulation of fat in the liver, can be classified into two primary categories: Non-Alcoholic Fatty Liver Disease (NAFLD) and Alcoholic Fatty Liver Disease (AFLD). Each of these categories includes specific subtypes and variations based on the underlying causes and the severity of liver damage.
1. Non-Alcoholic Fatty Liver Disease (NAFLD)
NAFLD is the most common form of chronic liver disease worldwide, especially in developed countries. It occurs in individuals who consume little to no alcohol and is closely linked to obesity, insulin resistance, and metabolic syndrome. NAFLD encompasses a spectrum of liver conditions:
- Simple Fatty Liver (Steatosis): This is the mildest form of NAFLD, where fat accumulates in the liver cells, but there is minimal or no inflammation or liver cell damage. Simple steatosis is generally considered benign, but it can progress to more severe conditions.
- Non-Alcoholic Steatohepatitis (NASH): NASH is a more severe form of NAFLD characterized by inflammation and damage to liver cells. This inflammation can lead to fibrosis (scarring) of the liver tissue, which increases the risk of developing cirrhosis, liver failure, or liver cancer.
2. Alcoholic Fatty Liver Disease (AFLD)
AFLD is caused by excessive alcohol consumption, which can lead to fat accumulation in the liver. The liver is responsible for breaking down alcohol, but excessive amounts can overwhelm the liver’s ability to process it, leading to fat buildup and inflammation. AFLD includes the following stages:
- Alcoholic Steatosis: The initial stage of AFLD, where fat starts accumulating in the liver cells due to excessive alcohol intake. This stage is often reversible with alcohol cessation.
- Alcoholic Hepatitis: This stage involves liver inflammation and damage, which can lead to symptoms such as jaundice, abdominal pain, and fever. Alcoholic hepatitis can be life-threatening if severe.
- Alcoholic Cirrhosis: The final stage of AFLD, where extensive fibrosis and scarring of the liver tissue occur. Cirrhosis significantly impairs liver function and increases the risk of liver failure, liver cancer, and other complications.
3. Other Types and Variants
There are also less common forms and subtypes of fatty liver disease, including:
- Pediatric NAFLD: Fatty liver disease is not limited to adults; it can also occur in children and adolescents. Pediatric NAFLD is often associated with obesity and metabolic syndrome in younger populations.
- Acute Fatty Liver of Pregnancy (AFLP): A rare but serious condition that occurs in pregnant women, usually in the third trimester. AFLP can lead to severe liver dysfunction and requires immediate medical attention.
- Drug-Induced Fatty Liver: Certain medications and toxins can cause fat accumulation in the liver. This condition is reversible upon discontinuation of the offending agent.
- Genetic and Metabolic Causes: Some genetic disorders and metabolic conditions, such as lipodystrophy and Wilson’s disease, can lead to fatty liver disease.
Causes and Risk Factors
The exact cause of fatty liver disease is not well understood, but several factors can increase the risk:
- Obesity: Excess body fat, particularly around the abdomen, is a significant risk factor.
- Insulin Resistance: Often associated with type 2 diabetes and metabolic syndrome, insulin resistance can lead to fat accumulation in the liver.
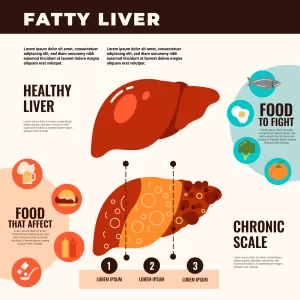
- High Fat Diet: Diets high in saturated fats, trans fats, and refined sugars can contribute to fatty liver.
- Alcohol Consumption: Heavy drinking can cause AFLD, while even moderate drinking can exacerbate NAFLD.
- Genetics: A family history of liver disease can increase susceptibility.
- Medications and Toxins: Certain medications and environmental toxins can contribute to liver fat accumulation.
Symptoms of Fatty Liver Disease
Fatty liver disease often develops silently, especially in its early stages. Many people with the condition may not experience noticeable symptoms until the disease progresses. When symptoms do occur, they can vary depending on the type and severity of the disease. Here’s a breakdown of common symptoms associated with different stages and types of fatty liver disease:
1. Non-Alcoholic Fatty Liver Disease (NAFLD)
- Simple Fatty Liver (Steatosis):
- Often asymptomatic
- Fatigue
- Mild discomfort or pain in the upper right abdomen
- Non-Alcoholic Steatohepatitis (NASH):
- Symptoms are more likely to appear compared to simple steatosis
- Persistent fatigue and tiredness
- Discomfort or pain in the upper right abdomen
- Unexplained weight loss
- Weakness
- Possible enlargement of the liver (hepatomegaly)
2. Alcoholic Fatty Liver Disease (AFLD)
- Alcoholic Steatosis:
- Frequently asymptomatic, particularly in the early stages
- Possible discomfort or pain in the upper right abdomen
- Alcoholic Hepatitis:
- Symptoms become more pronounced
- Fever
- Jaundice (yellowing of the skin and eyes)
- Nausea and vomiting
- Abdominal pain and tenderness, particularly in the upper right side
- Loss of appetite
- Fatigue
- Dark urine
- Pale stools
- Alcoholic Cirrhosis:
- Symptoms of liver failure and complications
- Severe fatigue and weakness
- Jaundice
- Abdominal swelling (ascites) due to fluid buildup
- Swelling in the legs and ankles (edema)
- Enlarged spleen (splenomegaly)
- Itchy skin
- Bruising and bleeding easily
- Confusion or difficulty thinking (hepatic encephalopathy)
- Weight loss
- Muscle wasting
3. Other Forms and Conditions Related to Fatty Liver Disease
- Pediatric NAFLD:
- Often asymptomatic
- May include fatigue and right upper abdominal discomfort
- Possible insulin resistance and signs of metabolic syndrome
- Acute Fatty Liver of Pregnancy (AFLP):
- Nausea and vomiting
- Abdominal pain, particularly in the upper right quadrant
- Jaundice
- Severe fatigue
- Headache
- Altered mental state or confusion
- Dark urine and pale stools
- Drug-Induced Fatty Liver:
- Symptoms depend on the drug and the extent of liver damage
- May include general fatigue and abdominal discomfort
Importance of Early Detection
Since fatty liver disease can progress to more serious conditions like cirrhosis, liver failure, or liver cancer, early detection and treatment are crucial. If you experience any persistent or unexplained symptoms, especially those related to liver function, it’s important to consult with a healthcare professional for a proper diagnosis and management plan.
Diagnosis
Diagnosing fatty liver disease involves a combination of assessing a patient’s medical history, physical examination, and various diagnostic tests. Since fatty liver disease often presents without symptoms, it is frequently detected incidentally during routine medical check-ups or evaluations for other conditions. Here’s an overview of the key methods used to diagnose fatty liver disease:
1. Medical History and Physical Examination
- Medical History:
- The doctor will inquire about the patient’s medical history, including any known risk factors such as obesity, diabetes, high cholesterol, or heavy alcohol consumption.
- A family history of liver disease or metabolic disorders will also be considered.
- Questions about the patient’s diet, exercise habits, and medication use are typically included.
- Physical Examination:
- The doctor may perform a physical examination to check for signs of liver disease, such as an enlarged liver (hepatomegaly) or jaundice (yellowing of the skin and eyes).
- Abdominal tenderness, particularly in the upper right quadrant, may also be assessed.
2. Blood Tests
Blood tests are a critical component of diagnosing fatty liver disease. They help assess liver function and detect any abnormalities:
- Liver Function Tests (LFTs): These tests measure the levels of liver enzymes (such as ALT, AST, ALP, and GGT), bilirubin, and proteins in the blood. Elevated liver enzymes can indicate liver inflammation or damage.
- Complete Blood Count (CBC): This test evaluates overall health and detects infections, anemia, and other disorders.
- Lipid Profile: Measures cholesterol and triglyceride levels, which can be elevated in fatty liver disease.
- Fasting Blood Sugar and HbA1c: These tests assess blood sugar levels and can indicate diabetes or insulin resistance, common in NAFLD.
- Serologic Tests for Hepatitis: These tests check for viral infections such as hepatitis B and C, which can also cause liver damage.
3. Imaging Studies
Imaging studies help visualize the liver and detect fat accumulation or other abnormalities:
- Ultrasound: This is often the first imaging test performed. It can detect fatty infiltration in the liver and assess liver size and texture. It is non-invasive and widely available.
- Computed Tomography (CT) Scan: A CT scan provides detailed images of the liver and can help identify fat, inflammation, fibrosis, or other structural changes.
- Magnetic Resonance Imaging (MRI): MRI provides high-resolution images and can be used to assess the extent of fat deposition and liver inflammation. It is particularly useful in distinguishing between simple steatosis and NASH.
- FibroScan (Transient Elastography): This non-invasive test measures liver stiffness, which can indicate fibrosis or cirrhosis. It is often used to assess the severity of liver disease.
4. Liver Biopsy
A liver biopsy is considered the gold standard for diagnosing and staging fatty liver disease, particularly for distinguishing between simple steatosis and NASH:
- Procedure: During a liver biopsy, a small needle is inserted through the skin to remove a tiny sample of liver tissue. The tissue is then examined under a microscope for signs of fat, inflammation, fibrosis, or other abnormalities.
- Indications: A liver biopsy may be recommended if there is uncertainty about the diagnosis or if non-invasive tests suggest significant liver damage.
5. Other Tests
- Genetic Testing: In cases where there is a family history of liver disease or other genetic conditions, genetic testing may be conducted to identify specific hereditary factors.
- Tests for Metabolic Disorders: Additional tests may be performed to rule out or confirm the presence of metabolic disorders that can contribute to fatty liver disease.
Importance of Comprehensive Diagnosis
A comprehensive and accurate diagnosis is essential for determining the appropriate treatment and management plan for fatty liver disease. Early diagnosis can help prevent the progression to more severe liver damage, such as fibrosis, cirrhosis, or liver cancer. If you have risk factors or symptoms of fatty liver disease, consult with a healthcare professional for a thorough evaluation.
Treatment of Fatty Liver Disease
Here’s a comprehensive look at the various treatment strategies for fatty liver disease:
1. Lifestyle Modifications
Lifestyle changes are the cornerstone of treatment for both Non-Alcoholic Fatty Liver Disease (NAFLD) and Alcoholic Fatty Liver Disease (AFLD). These changes can significantly reduce liver fat, inflammation, and the risk of complications:
- Weight Loss: Losing weight is crucial for patients with NAFLD, especially if they are overweight or obese. A weight loss of 5-10% of body weight can lead to significant improvements in liver health, including reduced liver fat, inflammation, and fibrosis.
- Healthy Diet: A balanced, nutritious diet is essential. Key dietary recommendations include:
- Reducing the intake of saturated fats, trans fats, and refined sugars.
- Increasing consumption of fruits, vegetables, whole grains, lean proteins, and healthy fats (such as those found in olive oil, nuts, and fatty fish).
- Considering a Mediterranean diet, which is rich in healthy fats, lean proteins, and fiber, and has been shown to benefit liver health.
- Regular Exercise: Physical activity helps reduce liver fat and improve overall metabolic health. A combination of aerobic exercises (such as walking, cycling, or swimming) and resistance training is recommended.
- Avoiding Alcohol: For those with AFLD, complete abstinence from alcohol is necessary to prevent further liver damage. Even those with NAFLD should limit or avoid alcohol intake, as it can exacerbate liver damage.
- Managing Comorbidities: Controlling other health conditions, such as diabetes, high blood pressure, and high cholesterol, is important for overall health and reducing liver disease progression.
2. Medications and Medical Treatments
Currently, there are no FDA-approved medications specifically for treating NAFLD or NASH. However, certain medications may be prescribed to manage symptoms, reduce liver inflammation, or treat associated conditions:
- Insulin Sensitizers: Medications such as metformin may be used to improve insulin sensitivity, especially in patients with type 2 diabetes or insulin resistance.
- Lipid-Lowering Agents: Statins and other lipid-lowering medications can help manage high cholesterol and triglyceride levels, reducing the risk of cardiovascular disease, which is often associated with NAFLD.
- Vitamin E and Antioxidants: Vitamin E, an antioxidant, has been studied for its potential benefits in reducing liver inflammation and fibrosis in NASH patients. However, its use should be carefully considered and discussed with a healthcare provider
.
NATURELO Vitamin E – 180 mg (300 IU) of Natural Mixed Tocopherols from Organic Whole Foods – Supplement for Healthy Skin, Hair, Nails, Immune & Eye Health – Non-GMO, Soy Free – 90 Vegan Capsules

Order Now
- Obeticholic Acid: This medication is being researched as a potential treatment for NASH, as it may reduce liver fibrosis.
- Other Medications: Depending on individual needs, doctors may prescribe other medications to manage symptoms or associated conditions, such as antihypertensive drugs or antidiabetic agents.
3. Surgical and Interventional Treatments
In certain cases, more aggressive treatments may be necessary:
- Bariatric Surgery: For individuals with severe obesity and NAFLD or NASH, bariatric surgery can lead to significant weight loss and improvement in liver health. Surgery is typically considered when lifestyle changes and medications are insufficient.
- Liver Transplant: In cases of advanced liver disease, such as cirrhosis or liver failure, a liver transplant may be the only viable option. This is considered when other treatments have failed, and the patient’s quality of life is severely compromised.
4. Regular Monitoring and Follow-up
Regular medical check-ups are essential for monitoring liver health and managing any complications:
- Liver Function Tests (LFTs): These are used to monitor liver enzyme levels and assess the liver’s condition.
- Imaging Studies: Periodic ultrasounds, CT scans, or MRIs may be used to monitor liver fat and fibrosis.
- FibroScan or Biopsy: These tests may be repeated periodically to assess liver stiffness and fibrosis, especially in patients with NASH or advanced liver disease.
5. Patient Education and Support
Educating patients about their condition, the importance of lifestyle changes, and adherence to medical treatments is crucial for successful management. Support groups and counseling can also help patients cope with the challenges of managing a chronic condition like fatty liver disease.
Prevention
Preventing fatty liver disease involves adopting a healthy lifestyle:
- Maintain a Healthy Weight: Aim for a balanced diet and regular exercise.
- Eat a Balanced Diet: Focus on whole grains, lean proteins, healthy fats, fruits, and vegetables.
- Avoid Alcohol or Drink in Moderation: Limit alcohol intake to reduce the risk of liver damage.
- Regular Check-ups: Regular medical check-ups can help detect liver issues early.
Conclusion
Fatty liver disease is a growing concern, but it is often preventable and manageable with the right lifestyle changes. By maintaining a healthy weight, eating a balanced diet, and exercising regularly, you can reduce your risk of developing this condition. If you suspect you have fatty liver disease, consult with a healthcare professional for appropriate diagnosis and treatment. Remember, early intervention can prevent more serious liver damage and improve your overall health.
Candi Liver Cleanse Support Supplement – Balance Control Probiotic Complex Cleanser for Women & Men – Oral Herbal Oregano & Caprylic Acid Capsules, Gallbladder Care Capsules & Milk Thistle Dandelion
The supplement contains a blend of ingredients such as probiotics, herbal extracts like oregano and milk thistle, caprylic acid, and others, which are often included for their potential benefits in supporting liver function and overall digestive health.
- Probiotics: These are beneficial bacteria that can help support gut health, which is closely linked to overall wellness, including liver health.
- Oregano: Known for its antimicrobial properties, oregano may help support a healthy balance of gut flora.
- Caprylic Acid: Often used for its antifungal properties, particularly in the context of combating yeast overgrowth.
- Milk Thistle: A well-known liver support herb, milk thistle is believed to help protect the liver from toxins and promote its regeneration.
- Dandelion: Often used for its diuretic properties, dandelion can help support the body’s natural detoxification processes.
Before starting any new supplement, especially for liver or gallbladder health, it’s a good idea to consult with a healthcare professional to ensure it’s safe and appropriate for your individual health needs.




