Sore Throat Showdown: Pharyngitis vs. Tonsillitis
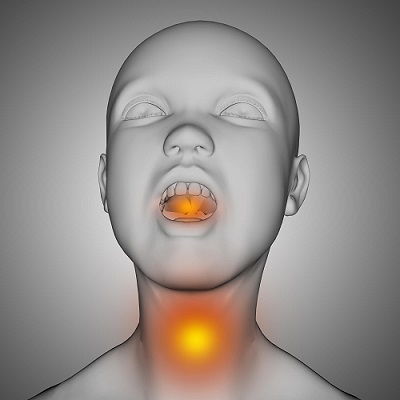
Tonsillitis and pharyngitis are two prevalent throat conditions that can cause significant discomfort and affect daily activities. Tonsillitis is the inflammation of the tonsils, while pharyngitis refers to the inflammation of the pharynx, the part of the throat behind the mouth and nasal cavity. Both conditions can lead to symptoms such as sore throat, difficulty swallowing, and fever, but they have distinct causes and treatments. Understanding these conditions, their symptoms, diagnosis, management, and prevention is essential for effective care and recovery.
Inflammation Fighters: The Pharynx and Tonsils
Before diving in, let’s meet the key players in your throat:
- Pharynx: This is the muscular tube at the back of your nose and mouth that connects to your esophagus (food tube) and windpipe (airway).
- Tonsils: These are two pad-like tissues located at the back of your throat, part of your body’s germ-fighting system.
Causes:
Tonsillitis
Etiology:
- Viral Infections: The most common cause of tonsillitis. Viruses that can cause tonsillitis include:
- Adenoviruses
- Influenza virus
- Epstein-Barr virus (EBV)
- Enteroviruses
- Respiratory syncytial virus (RSV)
- Coronaviruses, including SARS-CoV-2 (COVID-19)
- Bacterial Infections: Bacteria can also cause tonsillitis, with Group A Streptococcus (GAS) being the most common bacterial cause.
- Streptococcus pyogenes (Group A Streptococcus)
- Less commonly, other bacteria such as:
- Staphylococcus aureus
- Streptococcus pneumoniae
- Haemophilus influenzae
- Moraxella catarrhalis
- Other Factors:
- Chronic tonsillitis may be associated with persistent bacterial colonization.
- Environmental factors, such as exposure to pollutants and allergens, can contribute to recurrent tonsillitis.
Pharyngitis
Etiology:
- Viral Infections: The majority of pharyngitis cases are viral in origin.
- Rhinoviruses
- Adenoviruses
- Influenza virus
- Parainfluenza virus
- Coronaviruses, including SARS-CoV-2
- Epstein-Barr virus (infectious mononucleosis)
- Herpes simplex virus
- Bacterial Infections: Bacterial causes are less common but important, especially in children.
- Group A Streptococcus (Streptococcus pyogenes), which can lead to streptococcal pharyngitis (strep throat)
- Group C and G Streptococcus
- Arcanobacterium haemolyticum
- Mycoplasma pneumoniae
- Chlamydia pneumoniae
- Neisseria gonorrhoeae (rare)
- Non-Infectious Causes:
- Allergies and irritants, such as smoke, pollution, and dry air, can cause pharyngitis.
- Gastroesophageal reflux disease (GERD) can lead to throat irritation and inflammation.
- Overuse of the voice (vocal strain) can result in pharyngitis.
Signs and Symptoms:
Both pharyngitis and tonsillitis cause a sore throat, but some symptoms can offer clues to the culprit:
Tonsillitis
- Swollen Tonsils: Noticeably larger than usual, often red.
- Sore Throat: Persistent pain that can make swallowing difficult.
- White or Yellow Coating: Spots or coating on the tonsils.
- Fever: Elevated body temperature.
- Bad Breath: Halitosis due to infection.
- Swollen Lymph Nodes: Tender nodes in the neck.
- Hoarseness: Changes in voice or difficulty speaking.
Pharyngitis
- Sore Throat: Painful, scratchy sensation in the throat.
- Red Pharynx: Visible redness in the throat area.
- Difficulty Swallowing: Pain while eating or drinking.
- Fever: Common in both viral and bacterial infections.
- Headache: Often accompanies the infection.
- Swollen Lymph Nodes: Tender nodes in the neck.
- Cough: Can be present, especially if caused by a virus.
- Runny Nose: Common with viral pharyngitis.
Diagnosis
- Physical Examination: Doctors look at the throat, tonsils, and neck.
- Throat Swab: A sample taken to test for bacterial infections like strep throat.
- Blood Tests: Sometimes necessary to rule out other conditions or confirm viral infections.
- Rapid Strep Test: Provides quick results for streptococcal bacteria.
- Complete Blood Count (CBC): Helps distinguish between bacterial and viral infections.
Tonsil Grading Chart
Tonsil grading is a way to assess the size of the tonsils, particularly in the context of conditions like tonsillitis and obstructive sleep apnea. The grading system helps healthcare providers determine the severity of tonsillar hypertrophy and the potential need for intervention. The grading is typically done on a scale from 0 to 4, based on how much of the oropharyngeal space the tonsils occupy.
| Grade | Description | Oropharyngeal Space Occupied |
|——- |———————————————- |———————————————|
| 0 | Tonsils are absent (post-tonsillectomy) | 0% |
| 1 | Tonsils within tonsillar pillars | <25% |
| 2 | Tonsils extend beyond tonsillar pillars | 25% – 50% |
| 3 | Tonsils beyond pillars, not reaching midline | 50% – 75% |
| 4 | Tonsils touch or nearly touch at midline | 75% – 100%
Clinical Implications
- Grade 0-1: Usually, no significant airway obstruction. Often considered normal or minor hypertrophy.
- Grade 2: Mild to moderate enlargement that may cause mild symptoms, such as snoring or minor swallowing difficulties.
- Grade 3: Moderate to severe enlargement that can cause more pronounced symptoms, including frequent throat infections, significant snoring, and potential sleep apnea.
- Grade 4: Severe enlargement, often associated with major symptoms like obstructive sleep apnea, significant swallowing difficulties, and frequent or chronic throat infections. Surgical intervention (tonsillectomy) is commonly considered.
Use in Clinical Practice
Healthcare providers use the tonsil grading chart during physical examinations, particularly when assessing children for conditions like recurrent tonsillitis or obstructive sleep apnea. The grading helps guide treatment decisions, including the consideration of surgery.
Management
Tonsillitis
- Rest: Ensuring adequate rest for recovery.
- Hydration: Drinking plenty of fluids to stay hydrated.
- Pain Relievers: Over-the-counter medications like ibuprofen or acetaminophen.
- Antibiotics: Prescribed if bacterial infection is confirmed.
- Saltwater Gargle: Can soothe a sore throat.
- Throat Lozenges: Provide temporary relief.
- Tonsillectomy: In recurrent or chronic cases, surgical removal of the tonsils may be recommended.
Pharyngitis
- Rest: Important to allow the body to fight the infection.
- Hydration: Essential to keep the throat moist and aid recovery.
- Pain Relievers: Medications such as acetaminophen or ibuprofen for pain and fever.
- Antibiotics: Only if bacterial infection like strep throat is confirmed.
- Throat Lozenges and Sprays: Can help soothe throat pain.
- Avoid Irritants: Such as smoking or polluted air, which can worsen symptoms.
- Humidifier: Using a humidifier can keep the throat from drying out.
Prevention
- Good Hygiene: Regular handwashing to prevent the spread of infections.
- Avoid Sharing Personal Items: Like utensils, to reduce transmission.
- Covering Mouth and Nose: Using tissues or elbows when coughing or sneezing.
- Stay Hydrated: Keeping mucous membranes moist and healthy.
- Healthy Diet: A balanced diet to support the immune system.
- Avoid Close Contact: With infected individuals to minimize risk.
- Vaccinations: Staying up to date with flu shots and other vaccines.

Flu Vaccine - Avoid secondhand smoke: Smoke irritates the throat and makes you more susceptible to infections.
- Get enough sleep: Adequate sleep strengthens your immune system, which helps fight off infections.
- Minimize stress: Chronic stress can weaken your immune system.
Conclusion
Both tonsillitis and pharyngitis, though uncomfortable, are manageable with proper care and attention. Early diagnosis and treatment are key to preventing complications. Maintaining good hygiene and a healthy lifestyle can significantly reduce the risk of these infections. By understanding the differences and similarities between these conditions, one can better navigate the symptoms and seek appropriate medical care.
Remember, this blog is for informational purposes only and shouldn’t replace consulting a healthcare professional. If you experience a sore throat, especially with a high fever or difficulty swallowing, see your doctor for proper diagnosis and treatment.
Frequently Asked Questions (FAQs) ;
Tonsillitis is the inflammation of the tonsils, while pharyngitis is the inflammation of the pharynx, the area of the throat behind the mouth and nasal cavity. Both can cause sore throat but involve different parts of the throat.
Symptoms include swollen tonsils, sore throat, white or yellow coating on the tonsils, fever, bad breath, swollen lymph nodes, and hoarseness.
Symptoms include a sore throat, red pharynx, difficulty swallowing, fever, headache, swollen lymph nodes, cough, and runny nose.
Diagnosis typically involves a physical examination, throat swab, rapid strep test, and sometimes blood tests like a complete blood count (CBC) to determine if the infection is viral or bacterial
Both conditions can be caused by viral or bacterial infections. Common viruses include the common cold and flu, while bacterial causes include Streptococcus pyogenes (strep throat).
Treatment may involve rest, hydration, pain relievers (e.g., ibuprofen, acetaminophen), throat lozenges, saltwater gargles, and antibiotics if a bacterial infection is confirmed. Severe or recurrent tonsillitis may require a tonsillectomy.
Yes, practicing good hygiene such as regular handwashing, avoiding sharing personal items, covering the mouth and nose when coughing or sneezing, staying hydrated, and maintaining a healthy diet can help prevent these infections.
Yes, tonsillitis can be contagious, especially if it is caused by a viral or bacterial infection. It can spread through respiratory droplets from coughing or sneezing, or by sharing utensils and personal items.
You should see a doctor if you have a severe sore throat, difficulty swallowing, high fever, swollen lymph nodes, white or yellow spots on the tonsils, or if symptoms persist for more than a few days. Also, seek medical advice if you experience recurrent infections.
If left untreated, both conditions can lead to complications such as abscess formation, spread of infection to nearby tissues, rheumatic fever, and kidney inflammation. Early treatment is important to prevent these outcomes.
Yes, allergies can cause pharyngitis. Allergens can irritate the throat and lead to inflammation.
Home remedies include drinking warm liquids, using a humidifier, gargling with salt water, sucking on throat lozenges, and ensuring adequate rest. These can help alleviate symptoms and support recovery. What is the difference between tonsillitis and pharyngitis?
What are common symptoms of tonsillitis?
What are common symptoms of pharyngitis?
How are tonsillitis and pharyngitis diagnosed?
What causes tonsillitis and pharyngitis?
How are tonsillitis and pharyngitis treated?
Can tonsillitis or pharyngitis be prevented?
Is tonsillitis contagious?
When should I see a doctor for tonsillitis or pharyngitis?
What complications can arise from untreated tonsillitis or pharyngitis?
Can allergies cause pharyngitis?
Are there any home remedies for tonsillitis and pharyngitis?



