Introduction
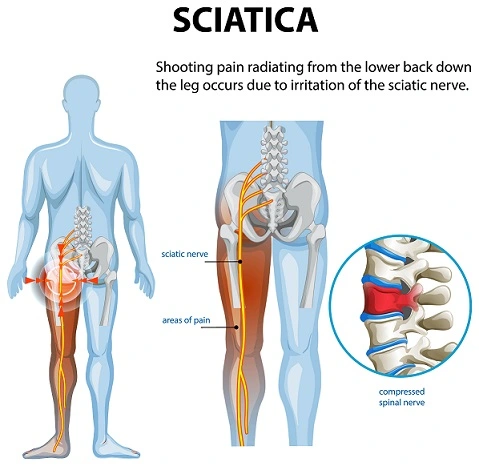
Sciatica affects up to 40% of adults at some point in their lives, making it one of the most common causes of lower back and leg pain. Characterized by pain radiating along the sciatic nerve (from the lower back through the hips and down each leg), sciatica can disrupt daily life and limit mobility. Whether you’re experiencing a dull ache or sharp, shooting pain, understanding sciatica is the first step toward effective management. In this guide, we’ll explore its causes, symptoms, treatments, and practical strategies to reclaim your comfort and mobility.
Signs and Symptoms :
Sciatica occurs when the sciatic nerve—the longest nerve in the body, running from the lower back down each leg—becomes compressed or irritated. The symptoms can range from mild discomfort to severe, debilitating pain. Here’s what to watch for:
Common Symptoms
✅ Radiating Pain – A sharp, burning, or electric-like pain that travels from the lower back through the buttock and down one leg (rarely both legs).
✅ Numbness or Tingling – A “pins and needles” sensation, often in the leg or foot.
✅ Muscle Weakness – Difficulty lifting the foot (foot drop) or weakness when moving the leg.
✅ Worsening with Movement – Pain may intensify when sitting, coughing, sneezing, or bending.
✅ Localized Lower Back Pain – Some people experience aching in the lower back along with leg pain.
Severe Red Flag Symptoms (Seek Immediate Medical Attention)
⚠️ Loss of Bladder/Bowel Control – Could indicate cauda equina syndrome, a rare but serious condition requiring emergency care.
⚠️ Sudden Severe Weakness – Inability to move the leg or foot.
⚠️ Progressive Numbness – Spreading numbness in the inner thighs or genital area.
Why Do These Symptoms Occur?
Sciatica is commonly caused by:
- Herniated or Bulging Discs (pressing on the nerve)
- Spinal Stenosis (narrowing of the spinal canal)
- Piriformis Syndrome (tight buttock muscles irritating the nerve)
- Spondylolisthesis (vertebrae slipping out of place)
If symptoms persist beyond 6 weeks or worsen, consult a doctor for imaging (MRI or CT scan) to confirm the diagnosis.
Diagnosis :
Sciatica symptoms can mimic other conditions, so proper diagnosis is crucial for effective treatment. Here’s how healthcare providers determine if your pain is truly sciatica—and what’s causing it.
1. Medical History & Physical Exam
Your doctor will first ask about:
✔ Pain location (Does it shoot down one leg?)
✔ Triggers (Does sitting, coughing, or bending worsen it?)
✔ Duration (Acute vs. chronic pain)
✔ Red flags (Loss of bladder control, severe weakness)
Common Physical Tests:
- Straight Leg Raise Test – Lying down, your doctor lifts your leg to see if it reproduces sciatic pain.
- Reflex, Strength & Sensation Checks – Tests for nerve dysfunction (e.g., weak ankle movement).
http://How to Prepare for a Back Pain Doctor’s Visit
2. Imaging Tests (If Needed)
If symptoms persist or worsen, your doctor may order:
MRI (Magnetic Resonance Imaging)
- Best for: Detecting herniated discs, spinal stenosis, or nerve compression.
- Why it’s used: Provides detailed images of soft tissues (nerves, discs).
CT Scan (Computed Tomography)
- Best for: Bone-related issues (fractures, arthritis).
- May include: A myelogram (dye injected into the spine for clearer nerve imaging).
X-Rays
- Limitation: Can’t show nerve damage but rules out fractures or tumors.
https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/ct-vs-mri-vs-xray
3. Nerve Tests (In Rare Cases)
If nerve damage is suspected:
- Electromyography (EMG) – Measures electrical activity in muscles.
- Nerve Conduction Study – Checks how well nerves send signals.
When to Seek Further Testing
🚩 Immediate imaging may be needed if you have:
- Sudden severe weakness
- Loss of bladder/bowel control
- Unexplained weight loss (possible tumor)
For mild cases, doctors often recommend 6 weeks of conservative treatment (rest, PT, meds) before ordering scans.
Key Takeaways
🔹 Most cases are diagnosed through history + physical exam.
🔹 MRI is the gold standard for nerve-related sciatica.
🔹 Nerve tests are rare but used for severe/atypical cases.
Next Steps: If you’re experiencing sciatica symptoms, start with a primary care visit. Early diagnosis leads to better outcomes!
🔴 Aggravating Factors: What Makes Sciatica Worse
1. Prolonged Sitting
- Why? Sitting increases pressure on the sciatic nerve by 40% compared to standing.
- Examples: Office jobs, long car rides, or excessive couch time.
- Fix: Use a lumbar support pillow and take breaks every 30 minutes.
2. Poor Posture
- Why? Slouching or hunching compresses spinal discs, irritating the nerve.
- Worst Offenders:
- Leaning forward at a desk
- Sleeping in a fetal position
- Carrying heavy bags on one shoulder
3. Heavy Lifting & Twisting Motions
- Why? Sudden strain can herniate discs or inflame the piriformis muscle.
- High-Risk Activities:
- Improper weightlifting
- Gardening/bending sideways
- Lifting while twisting (e.g., moving boxes)
4. High-Impact Exercise
- Why? Running, jumping, or intense sports jar the spine.
- Alternatives: Swap for low-impact activities (swimming, walking).
5. Obesity & Sedentary Lifestyle
- Why? Excess weight strains the lower back, while inactivity weakens core muscles.
https://www.health.harvard.edu/blog/taming-pain-sciatica-people-time-heals-less-2017071212048
🟢 Relieving Factors: What Eases Sciatica Pain
1. Movement & Gentle Stretching
- Why? Walking loosens stiff muscles, while targeted stretches decompress the nerve.
- Best Exercises:
- Piriformis stretch (seated or lying)
- Cat-Cow yoga pose
- Pelvic tilts
2. Heat & Cold Therapy
- Ice Packs (first 48 hours of acute pain) – Reduces inflammation.
- Heating Pads (after 48 hours) – Relaxes tight muscles.
3. Ergonomic Adjustments
- Sleeping Position: On your side with a pillow between knees.
- Workstation: Monitor at eye level, feet flat on the floor.
4. Anti-Inflammatory Diet
- Top Foods: Turmeric, ginger, leafy greens, and omega-3s (salmon, walnuts).
5. Over-the-Counter (OTC) Pain Relief
- NSAIDs (ibuprofen) – Reduces swelling.
- Topical creams (menthol or capsaicin) – Blocks pain signals.
https://www.health.harvard.edu/pain/sciatica-home-remedies-and-self-care
⚠️ When to See a Doctor
If pain worsens despite rest or you experience:
- Numbness in the groin/butocks
- Leg weakness
- Bowel/bladder changes
Key Takeaways
✅ Avoid: Sitting >30 mins, heavy lifting, slouching.
✅ Do: Walk daily, use heat/ice, stretch gently.
✅ Emergency Signs: Leg weakness or loss of bladder control.
Pro Tip: Keep a pain diary to track triggers and share it with your doctor.
Sciatica Pain-Relieving Exercises (With Step-by-Step Images)
Sciatica pain often improves with targeted stretches and strengthening exercises. Below are 5 proven moves to relieve nerve pressure, reduce inflammation, and restore mobility.
🔹 1. Piriformis Stretch
Targets: The piriformis muscle (often compresses the sciatic nerve).
How to Do It:
- Lie on your back, bend both knees.
- Cross your affected leg’s ankle over the opposite knee.
- Gently pull the uncrossed leg toward your chest until you feel a stretch in the buttock.
- Hold for 30 seconds, then switch sides.
Tip: Keep your spine flat on the floor.
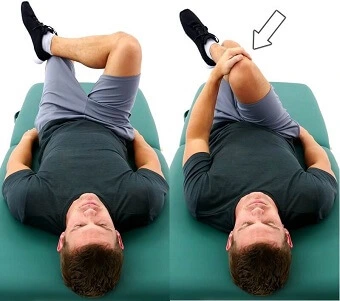
🔹 2. Knee-to-Chest Stretch
Relieves: Lower back tension pressing on the sciatic nerve.
How to Do It:
- Lie on your back, legs extended.
- Slowly pull one knee toward your chest, keeping the other leg straight.
- Hold for 20 seconds, then switch legs.
Avoid: Jerking motions—move slowly.
https://www.health.com/lower-back-stretches-for-back-pain-7504553
🔹 3. Cat-Cow Pose (Yoga for Sciatica)
Benefits: Mobilizes the spine and reduces nerve compression.
How to Do It:
- Start on hands and knees (tabletop position).
- Inhale: Arch your back (Cow Pose—belly down).
- Exhale: Round your spine (Cat Pose—chin to chest).
- Repeat for 1-2 minutes.
Tip: Sync movements with breathing.
https://www.healthline.com/health/yoga-for-sciatica#half-moon-pose
🔹 4. Pelvic Tilts
Strengthens: Core muscles to support the lower back.
How to Do It:
- Lie on your back, knees bent, feet flat.
- Tighten your abs and press your lower back into the floor.
- Hold for 5 seconds, then release.
- Repeat 10 times.

For Progression: Try bridging (lifting hips off the floor).
🔹 5. Seated Spinal Twist
Stretches: Glutes and lower back to decompress the nerve.
How to Do It:
- Sit on the floor, legs extended.
- Bend one knee and cross it over the opposite leg.
- Twist your torso toward the bent knee, using your arm for leverage.
- Hold for 20 seconds, then switch sides.

Caution: Don’t force the twist—go only as far as comfortable.
🚫 Exercises to Avoid with Sciatica
- Toe Touches (overstretches hamstrings, strains discs).
- Heavy Deadlifts (compresses spinal nerves).
- High-Impact Cardio (running, jumping).
📌 Key Tips for Success
✔ Warm up first (walk 5-10 minutes).
✔ Do stretches 2x daily (morning/night).
✔ Stop if pain shoots down the leg (gentle tension is okay).
For severe pain, consult a physical therapist.
💡 Did You Know?
Studies show consistent stretching reduces sciatica pain by 40% within 4 weeks.
Next Steps: Try these daily for 2 weeks and track your progress!
Effective Management of Sciatica:
Sciatica management involves a combination of medical treatments, physical therapy, lifestyle changes, and (in rare cases) surgery. The goal is to reduce pain, improve mobility, and prevent recurrence. Below, we outline the best evidence-based approaches.
1. Medical Treatments
✅ Medications
- NSAIDs (Ibuprofen, Naproxen) – Reduce inflammation and pain.
- Muscle Relaxants (Cyclobenzaprine) – Ease muscle spasms.
- Oral Steroids (Prednisone) – Short-term use for severe inflammation.
- Nerve Pain Medications (Gabapentin, Pregabalin) – For chronic nerve irritation.
https://www.spine-health.com/blog/medication-sciatica
✅ Epidural Steroid Injections
- Best for: Severe pain unresponsive to oral meds.
- How it works: Cortisone injected near the nerve to reduce swelling.
- Effect lasts: Weeks to months.
2. Physical Therapy & Exercise
A structured PT program strengthens core muscles, improves posture, and relieves nerve pressure.
Key Exercises:
- Piriformis Stretches
- Pelvic Tilts
- McKenzie Press-Ups (for disc-related sciatica)
- Low-Impact Aerobics (walking, swimming)
https://www.spine-health.com/conditions/sciatica/physical-therapy-and-exercise-sciatica
3. Alternative Therapies
✅ Chiropractic Adjustments
- Helps realign the spine and reduce nerve compression.
✅ Acupuncture
- May stimulate pain-relieving endorphins.
✅ Massage Therapy
- Focuses on piriformis muscle and lower back tension.
https://pmc.ncbi.nlm.nih.gov/articles/PMC4631886/
4. Lifestyle & Home Remedies
✅ Heat & Ice Therapy
- Ice (first 48 hours) – Reduces swelling.
- Heat (after 48 hours) – Relaxes tight muscles.
✅ Ergonomic Adjustments
- Use a lumbar support pillow when sitting.
- Sleep in a side position with a pillow between knees.
✅ Anti-Inflammatory Diet
- Foods like turmeric, ginger, and omega-3s may help.
5. Surgical Options (Last Resort)
Surgery is considered if:
- Pain persists > 6-12 weeks despite treatment.
- There’s severe weakness or loss of bladder control.
Common Procedures:
- Microdiscectomy – Removes herniated disc material pressing on the nerve.
- Laminectomy – Widens the spinal canal for stenosis-related sciatica.
🚫 What to Avoid with Sciatica
- Prolonged sitting (take breaks every 30 mins).
- Heavy lifting or twisting motions.
- High-impact exercises (running, jumping).
🔑 Key Takeaways
✔ 90% of sciatica cases improve without surgery.
✔ Movement (walking, stretching) is better than bed rest.
✔ Seek emergency care for sudden weakness or bladder issues.
Things to Avoid with Sciatica
- Prolonged Sitting: Take breaks every 30 minutes to stretch.
- Heavy Lifting: Use proper form or avoid altogether.
- High-Impact Activities: Running or jumping may worsen symptoms.
- Poor Footwear: Avoid high heels or unsupportive shoes.
- Ignoring Pain: Pushing through pain can lead to chronic issues.
Conclusion
Sciatica can be debilitating, but with the right approach, most people find relief within weeks. By combining targeted exercises, lifestyle adjustments, and professional care, you can reduce flare-ups and regain control. Always consult a healthcare provider for persistent pain, and remember: proactive management is key to long-term spinal health.
Final Takeaways:
- Early intervention prevents chronic sciatica.
- Stay active, but avoid overexertion.
- Prioritize ergonomics in daily routines.
FAQS,
What is sciatica?
Sciatica refers to pain that radiates along the path of the sciatic nerve, which branches from the lower back through the hips, buttocks, and down each leg. It usually affects one side of the body.
What causes sciatica?
The most common cause is a herniated (slipped) disc in the spine that presses on the sciatic nerve. Other causes include: - Spinal stenosis (narrowing of the spinal canal) - Piriformis syndrome (tightening of the piriformis muscle in the buttocks) - Spondylolisthesis (vertebra slipping out of place) - Injury or infection
What are the symptoms of sciatica?
- Sharp, burning, or shooting pain from the lower back to the leg - Numbness or tingling in the leg or foot - Weakness in the affected leg - Worsening pain when sitting, coughing, or sneezing
How is sciatica diagnosed?
A doctor may perform: - Physical examination (checking reflexes, muscle strength, and pain triggers) - Imaging tests (X-ray, MRI, or CT scan) to identify nerve compression
How is sciatica treated?
- Medications: Pain relievers (NSAIDs), muscle relaxants, or steroids - Physical therapy: Stretching and strengthening exercises - Hot/cold therapy: Reduces inflammation and pain - Epidural steroid injections: For severe pain - Surgery (in rare cases): Microdiscectomy or laminectomy
How long does sciatica last?
- Acute sciatica: Usually improves in 4-6 weeks with self-care. - Chronic sciatica: May last longer if underlying conditions persist.
Can sciatica be prevented?
- Maintain good posture - Exercise regularly (especially core- strengthening workouts) - Lift objects properly (bend at the knees, not the waist) - Avoid prolonged sitting
When should I see a doctor?
- Seek immediate medical help if you experience: - Severe pain or sudden weakness in the leg - Loss of bladder or bowel control (cauda equina syndrome—a medical emergency)
Can sciatica go away on its own?
Yes, mild cases often resolve with rest, stretching, and over-the-counter pain relief. However, recurring or severe cases need medical attention.
Are there home remedies for sciatica relief?
- Gentle stretches (e.g., knee-to-chest stretch, piriformis stretch) - Yoga or Pilates (improves flexibility and strength) - Massage therapy (reduces muscle tension) - Acupuncture or chiropractic care (may help some patients)



