Typhoid Fever: An In-Depth Overview
Typhoid fever is a serious and potentially life-threatening illness caused by the bacterium Salmonella enterica serotype Typhi. Despite advances in medicine, it remains a significant health concern, particularly in developing countries. This blog provides a comprehensive overview of typhoid fever, including its etiology, types, signs and symptoms, diagnosis, management, and prevention strategies.
Introduction
Typhoid fever is a systemic infection characterized by prolonged fever, abdominal pain, and a range of other symptoms. It primarily spreads through contaminated food and water, making it a prevalent issue in regions with poor sanitation and limited access to clean water. The World Health Organization estimates that typhoid fever affects 11-20 million people each year, resulting in approximately 128,000 to 161,000 deaths annually.
Etiology
The causative agent of typhoid fever is the bacterium Salmonella enterica serotype Typhi. This pathogen is highly adapted to humans and spreads primarily through the fecal-oral route. People become infected by consuming food or water contaminated with the feces of an infected person. Poor sanitation, inadequate hygiene practices, and limited access to clean water significantly contribute to the spread of this disease.
Types of Typhoid and Paratyphoid Fever
Typhoid fever and paratyphoid fever are systemic infections caused by different serotypes of the Salmonella bacterium. Understanding the distinctions between these types is crucial for diagnosis, treatment, and prevention.
1. Typhoid Fever
Causative Agent:
- Salmonella enterica serotype Typhi (S. Typhi)
Characteristics:
- Typhoid fever is the classic form of the disease, characterized by prolonged high fever, abdominal pain, and systemic symptoms.
- It is more severe and has a higher mortality rate if untreated compared to paratyphoid fever.
- S. Typhi is highly adapted to humans and does not have an animal reservoir, making human-to-human transmission via contaminated food and water the primary mode of spread.
2. Paratyphoid Fever
Causative Agents:
- Salmonella enterica serotype Paratyphi A (S. Paratyphi A)
- Salmonella enterica serotype Paratyphi B (S. Paratyphi B)
- Salmonella enterica serotype Paratyphi C (S. Paratyphi C)
Characteristics:
- Paratyphoid fever presents similarly to typhoid fever but is generally milder.
- It can still cause significant illness, particularly in individuals with compromised immune systems or in areas with high transmission rates.
- S. Paratyphi can be transmitted similarly to S. Typhi through contaminated food and water, with humans being the primary reservoir.
Key Differences Between Typhoid and Paratyphoid Fever
- Severity:
- Typhoid fever (caused by S. Typhi) tends to be more severe than paratyphoid fever.
- Geographic Distribution:
- Both types are prevalent in regions with poor sanitation, particularly in South Asia, Southeast Asia, Africa, and parts of South America. However, the prevalence of specific serotypes can vary geographically.
- Clinical Features:
- While both diseases share similar clinical features such as fever, abdominal pain, and systemic symptoms, paratyphoid fever may have a milder presentation and a shorter duration.
- Complications:
- Typhoid fever has a higher risk of complications such as intestinal perforation, hemorrhage, and severe systemic involvement.
- Incubation Period:
- Typhoid fever has an incubation period of 6-30 days, while paratyphoid fever typically has a slightly shorter incubation period of 1-10 days.
Signs and Symptoms
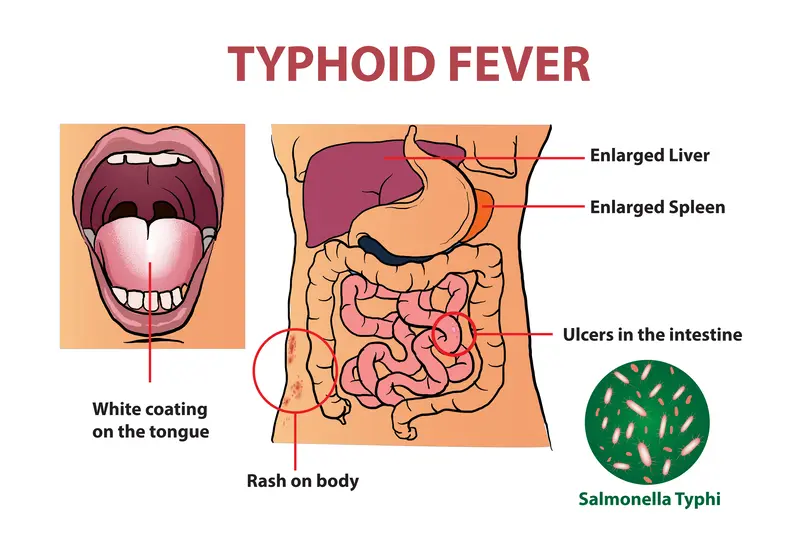
The symptoms of typhoid fever typically develop 6-30 days after exposure. The illness can present in various stages, with symptoms evolving over time:
- First Week:
- Gradual onset of fever, often increasing daily.
- Headache, malaise, and fatigue.
- Muscle aches and joint pain.
- Dry cough.
- Second Week:
- High fever, often peaking at 103-104°F (39-40°C).
- Abdominal pain and bloating.
- Rose-colored spots on the trunk.
- Diarrhea or constipation.
- Anorexia and weight loss.
- Third Week:
- Severe abdominal distension.
- Complications such as intestinal hemorrhage or perforation.
- Delirium and altered mental status.
- Fourth Week and Beyond:
- Gradual resolution of symptoms if untreated, but relapses can occur.
- Without treatment, severe complications can lead to death.
Diagnosis
Diagnosing typhoid fever involves a combination of clinical evaluation and laboratory tests. Early and accurate diagnosis is crucial for effective treatment and preventing complications.
1. Clinical Evaluation
Patient History:
- Obtain detailed information about the patient’s symptoms, duration of illness, and travel history, especially to endemic areas.
- Ask about exposure to potentially contaminated food or water and contact with known typhoid cases.
Physical Examination:
- Look for signs such as sustained high fever, abdominal tenderness, and hepatosplenomegaly (enlarged liver and spleen).
- Check for the presence of rose spots (small, pink maculopapular lesions) on the trunk and abdomen.
2. Laboratory Tests
Blood Culture:
- The gold standard for diagnosing typhoid fever, especially in the first week of illness.
- Blood samples are cultured to detect Salmonella Typhi or Paratyphi.
- Multiple blood cultures may be necessary to increase diagnostic yield.
Bone Marrow Culture:
- More sensitive than blood culture and can detect the bacteria even when patients have started antibiotics.
- Typically reserved for difficult cases or when blood cultures are negative.
Stool and Urine Culture:
- Useful but less reliable than blood cultures.
- Stool cultures may become positive after the first week of illness.
- Urine cultures are less commonly used due to lower sensitivity.
Typhoid rapid diagnostic tests:
These newer tests can detect S. typhi antigens or antibodies in blood or other body fluids within a few hours. However, they may not be as accurate as cultures and are not yet widely available.
Polymerase Chain Reaction (PCR):
- Highly sensitive and specific method for detecting Salmonella DNA in blood, stool, or other body fluids.
- Rapid and accurate but less commonly available in resource-limited settings.
Complete Blood Count (CBC):
- May show leukopenia (low white blood cell count), anemia, and thrombocytopenia (low platelet count), which are common in typhoid fever.
Liver Function Tests:
- May show elevated liver enzymes due to hepatic involvement in typhoid fever.
Imaging Studies
Abdominal Ultrasound or CT Scan:
- Not routinely used for diagnosis but can be helpful in evaluating complications such as intestinal perforation or abscess formation.
Differential Diagnosis
Typhoid fever shares symptoms with many other illnesses, so it’s crucial to differentiate it from other febrile illnesses such as:
- Malaria
- Dengue fever
- Tuberculosis
- Viral hepatitis
- Leptospirosis
- Brucellosis
Accurate diagnosis often requires ruling out these conditions through appropriate tests and clinical evaluation.
Management
Managing typhoid fever involves a combination of antimicrobial therapy, supportive care, and addressing complications if they arise. Early diagnosis and prompt treatment are critical to reducing morbidity and preventing complications.
1. Antimicrobial Therapy
First-Line Antibiotics:
- Ciprofloxacin: A fluoroquinolone commonly used for susceptible strains of Salmonella Typhi. However, resistance is increasing.
- Azithromycin: Effective against multidrug-resistant (MDR) strains. It is an alternative to fluoroquinolones.
- Ceftriaxone: A third-generation cephalosporin used for severe cases or when resistance to other antibiotics is suspected.
Alternative Antibiotics:
- Chloramphenicol, Ampicillin, and Trimethoprim-Sulfamethoxazole (TMP-SMX): Once common treatments, now less frequently used due to widespread resistance.
Treatment Duration:
- Uncomplicated cases typically require 7-14 days of antibiotic therapy.
- Severe or complicated cases may require extended courses, often up to 14-21 days.
2. Supportive Care
Hydration and Electrolyte Management:
- Oral rehydration solutions (ORS) or intravenous fluids to prevent dehydration and maintain electrolyte balance, especially in patients with severe diarrhea.
Nutritional Support:
- Adequate nutrition to support recovery. Small, frequent meals are recommended to ensure caloric intake.
Antipyretics:
- Paracetamol (acetaminophen) or ibuprofen to manage fever and alleviate discomfort.
Pain Management:
- Analgesics for abdominal pain and discomfort.
3. Hospitalization
Indications for Hospitalization:
- Severe cases with high fever, severe abdominal pain, or altered mental status.
- Complications such as gastrointestinal bleeding, perforation, or shock.
- Dehydration not manageable with oral rehydration.
4. Management of Complications
Intestinal Perforation:
- Surgical intervention may be required for repair.
- Broad-spectrum antibiotics to cover potential secondary infections.
Gastrointestinal Hemorrhage:
- Blood transfusions if necessary.
- Endoscopic or surgical interventions to control bleeding.
Sepsis and Septic Shock:
- Aggressive antibiotic therapy.
- Intravenous fluids and vasopressors for hemodynamic support.
Chronic Carrier State:
- Approximately 1-5% of patients become chronic carriers, excreting the bacteria in their stool for more than a year.
- Long-term antibiotic therapy (e.g., ciprofloxacin) or cholecystectomy (removal of the gallbladder) for persistent carriers.
5. Follow-Up Care
Monitoring for Relapse:
- Regular follow-up visits to monitor for relapse of symptoms, which can occur in about 5-10% of treated cases.
- Repeat cultures if symptoms recur.
Public Health Measures:
- Reporting cases to public health authorities for contact tracing and control measures.
- Educating patients on hygiene practices to prevent spread, especially if they are food handlers.
Prevention
Vaccination
Available Vaccines:
- Vi Polysaccharide Vaccine (Injectable): A single-dose vaccine given to individuals over two years of age.
- Live Attenuated Oral Vaccine (Ty21a): Given as a series of capsules over several days, suitable for individuals over six years of age.
Target Groups:
- Travelers to endemic areas.
- Populations in high-risk regions.
- Close contacts of typhoid carriers.
Public Health Interventions
Improving Sanitation:
- Ensuring access to clean water and proper sewage disposal.
- Promoting the use of latrines and safe waste management practices.
Hygiene Education:
- Educating communities about handwashing, safe food preparation, and the importance of boiling or treating drinking water.
Food Safety:
- Ensuring that food is cooked thoroughly and stored properly.
- Avoiding raw fruits and vegetables unless they can be peeled and are safe from contamination.
Global Impact
- Endemic Areas: Predominantly affects regions in South Asia, Southeast Asia, Africa, and parts of Latin America and the Caribbean.
- Burden of Disease: High morbidity and mortality rates in areas with poor sanitation infrastructure.
Challenges
- Antibiotic Resistance: Increasing resistance to commonly used antibiotics is a major challenge, necessitating continuous monitoring and development of new treatment protocols.
- Access to Healthcare: Limited access to medical care and diagnostic facilities in endemic regions hampers timely diagnosis and treatment.
Conclusion
Typhoid fever remains a significant public health challenge, particularly in areas with inadequate sanitation and limited access to clean water. Understanding the etiology, types, signs and symptoms, diagnosis, and management of typhoid fever is crucial for controlling its spread and reducing its impact on affected populations. Through improved sanitation, vaccination, and personal hygiene practices, the burden of typhoid fever can be significantly reduced, ultimately saving lives and improving health outcomes worldwide.
FAQs,
What is typhoid fever?
It is a bacterial infection caused by Salmonella enterica serotype Typhi. It is characterized by prolonged fever, abdominal pain, and other systemic symptoms. The infection spreads through contaminated food and water.
How is typhoid fever transmitted?
Typhoid fever is primarily transmitted through the fecal-oral route. This occurs when people consume food or water contaminated with the feces of an infected person. Poor sanitation and hygiene practices facilitate the spread of the disease.
What are the symptoms of typhoid fever?
Common symptoms include: High fever Abdominal pain Headache Weakness and fatigue Muscle aches Loss of appetite Diarrhea or constipation Rose-colored spots on the trunk
How is typhoid fever diagnosed?
Typhoid fever is diagnosed through a combination of: Blood cultures (gold standard) Stool and urine cultures Widal test (serological test for antibodies) Polymerase Chain Reaction (PCR) for detecting bacterial DNA Bone marrow culture (high sensitivity)
How is typhoid fever treated?
Typhoid fever is treated with antibiotics, including: Ciprofloxacin or other fluoroquinolones Azithromycin Ceftriaxone Supportive care, such as hydration, antipyretics, and nutritional support, is also essential. Severe cases may require hospitalization.
Can typhoid fever be prevented?
Yes, prevention strategies include: Vaccination: Injectable Vi polysaccharide vaccine and oral live-attenuated Ty21a vaccine. Improved sanitation: Access to clean water and proper sewage disposal. Hygiene practices: Regular handwashing, safe food preparation, and avoiding potentially contaminated food and water.
Who is at risk for typhoid fever?
People living in or traveling to areas with poor sanitation and limited access to clean water are at higher risk. This includes many parts of South Asia, Southeast Asia, Africa, and Latin America.
What are the complications of typhoid fever?
Potential complications include: Intestinal perforation Gastrointestinal hemorrhage Sepsis and septic shock Hepatosplenomegaly Delirium and altered mental status
How long does it take to recover from typhoid fever?
With appropriate antibiotic treatment, most patients begin to improve within a few days and recover fully within 1-2 weeks. However, without treatment, the illness can last for weeks or months and may lead to severe complications or death.
Can typhoid fever recur?
Yes, about 5-10% of patients may experience a relapse of symptoms after initial recovery. Continuous follow-up and complete antibiotic courses are crucial to prevent recurrence.
What is the chronic carrier state of typhoid fever?
Approximately 1-5% of people who recover from typhoid fever can become chronic carriers, excreting the bacteria in their stool for more than a year. Carriers can spread the disease even if they have no symptoms. Long-term antibiotics or surgical removal of the gallbladder may be required to eradicate the carrier state.
Is there a difference between typhoid fever and paratyphoid fever?
Yes, typhoid fever is caused by Salmonella enterica serotype Typhi, while paratyphoid fever is caused by Salmonella enterica serotypes Paratyphi A, B, and C. Paratyphoid fever typically has a milder presentation but shares many clinical features and transmission routes with typhoid fever.