Asthma, a chronic respiratory condition affecting millions worldwide, presents a unique challenge in managing daily life and maintaining respiratory health. This blog aims to shed light on asthma—its causes, symptoms, management strategies, and tips for living well with this condition.
What is Asthma?
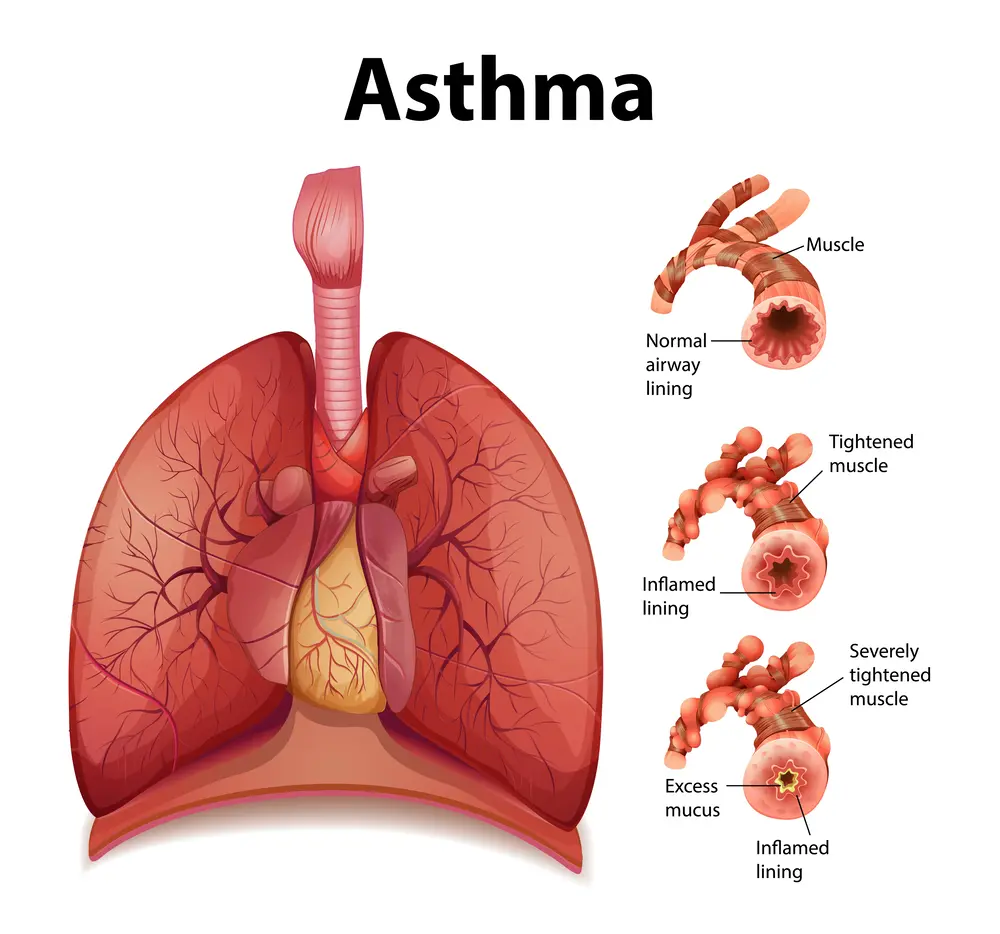
Asthma is a chronic disease that affects the airways in the lungs, making breathing difficult. It involves inflammation and narrowing of the airways, as well as increased sensitivity to various triggers. Common symptoms include wheezing, shortness of breath, chest tightness, and coughing, which can vary in severity and frequency from person to person.
Recognizing the Symptoms of Asthma
It symptoms can vary widely among individuals, but understanding the common signs is crucial for timely diagnosis and effective management. Here are the primary symptoms:
1. Wheezing
- Description: Wheezing is a high-pitched whistling sound that occurs when breathing, especially during exhalation.
- Significance: It is one of the most characteristic symptoms of asthma and results from the narrowing of the airways.
2. Shortness of Breath
- Description: Experiencing difficulty in breathing or feeling breathless, as if you cannot get enough air.
- Significance: This symptom can range from mild discomfort to severe difficulty in breathing, particularly during physical activity or at night.
3. Chest Tightness
- Description: A feeling of tightness, pressure, or constriction in the chest.
- Significance: Chest tightness is often a sign of an impending asthma attack and should be monitored closely.
4. Coughing
- Description: Persistent coughing that may worsen at night or early in the morning.
- Significance: Asthma-related coughing is typically dry and non-productive, though it can sometimes bring up mucus.
5. Increased Mucus Production
- Description: Excessive production of mucus in the airways.
- Significance: While not as common as other symptoms, increased mucus can contribute to airway obstruction and coughing.
6. Difficulty Sleeping
- Description: Trouble falling or staying asleep due to coughing, wheezing, or shortness of breath.
- Significance: Nocturnal asthma symptoms can significantly impact sleep quality and overall well-being.
7. Fatigue
- Description: Feeling unusually tired or fatigued, even with adequate rest.
- Significance: Chronic asthma symptoms can lead to fatigue due to the increased effort required to breathe and poor sleep quality.
When to Seek Medical Attention
It’s essential to seek medical advice if you experience any of the following:
- Symptoms that are frequent or persistent.
- Symptoms that worsen despite using prescribed medications.
- Difficulty breathing that does not improve with quick-relief inhalers.
- Severe asthmatic attacks that cause significant breathlessness or chest tightness.
Causes and Triggers
Several factors can contribute to the development and exacerbation of asthma:
- Genetics: Family history of asthma or allergies increases the risk.
- Allergens: Common triggers include pollen, dust mites, pet dander, mold, and certain foods.
- Environmental Factors: Air pollution, cigarette smoke, strong odors, and cold air can trigger symptoms.
- Respiratory Infections: Viral infections can worsen asthma symptoms.
- Physical Activity: Exercise-induced asthma can occur during or after physical exertion.
- Emotional Factors: Stress and strong emotions may trigger asthmatic attacks in some individuals.
Understanding personal triggers is crucial for managing asthma effectively and preventing flare-ups.
Diagnosis
It involves a systematic approach that includes medical history evaluation, physical examination, and diagnostic tests to confirm the presence of asthma and assess its severity. Here’s an overview of the diagnostic process:
1. Medical History
- Symptom Assessment: Your healthcare provider will inquire about your symptoms, including episodes of wheezing, shortness of breath, chest tightness, and coughing, especially at night or in response to triggers.
- Family History: Asthma and allergies tend to run in families, so your family history of asthma or allergic conditions is important.
- Triggers: Discuss potential triggers that worsen your symptoms, such as allergens, exercise, cold air, or respiratory infections.
2. Physical Examination
- Lung Function: Your doctor will listen to your lungs with a stethoscope to assess any abnormal sounds (like wheezing) and evaluate your overall respiratory function.
- Signs of Allergies: Skin or nasal congestion may indicate allergies that can contribute to asthma symptoms.
3. Diagnostic Tests
- Pulmonary Function Tests (PFTs):
- Spirometry: This common lung function test measures how much and how quickly you can exhale air. It helps assess the narrowing of your airways and how well your lungs are functioning.
- Peak Expiratory Flow (PEF) Measurement: PEF monitoring with a peak flow meter helps track changes in airflow and assesses the severity of asthma. It can be done at home to monitor daily lung function.
4. Additional Tests
- Bronchodilator Reversibility Test: After spirometry, you may inhale a bronchodilator medication (such as albuterol) to see if it improves airflow. A significant increase in lung function indicates asthma.
- Allergy Tests: If allergies are suspected triggers, skin or blood tests (like IgE antibody tests) may be performed to identify specific allergens.
- Exhaled Nitric Oxide Test: This test measures the level of nitric oxide in your breath, which can indicate airway inflammation associated with asthma.
5. Diagnosis Confirmation
- Asthma Diagnosis: Based on your medical history, symptoms, physical exam findings, and test results (especially spirometry showing reversible airflow obstruction), your healthcare provider will confirm a diagnosis of asthma.
6. Monitoring and Follow-Up
- Asthma Action Plan: Once diagnosed, your doctor will work with you to develop an asthma action plan. This personalized plan outlines daily treatment, identifies triggers to avoid, and provides steps to take during worsening symptoms or asthmatic attacks.
- Regular Follow-Up: It’s important to schedule regular follow-up appointments with your healthcare provider to monitor your asthma control, adjust treatment as needed, and review your asthma action plan.
Effective Management of Asthma: A Comprehensive Guide
Asthma is a chronic condition that requires diligent management to control symptoms, prevent exacerbations, and maintain a high quality of life. Here are key strategies and tips for effectively managing asthma:
1. Medications
There are two main types of asthma medications:
- Quick-Relief Medications:
- Short-Acting Beta-Agonists (SABAs): These inhalers, such as albuterol, provide rapid relief from acute symptoms by relaxing the muscles around the airways.
- Anticholinergics: Medications like ipratropium can help open the airways and reduce mucus production.
- Long-Term Control Medications:
- Inhaled Corticosteroids: These are the most effective long-term control medications. They reduce inflammation and prevent symptoms.
- Long-Acting Beta-Agonists (LABAs): These are often combined with inhaled corticosteroids for better control.

-
- Leukotriene Modifiers: These oral medications reduce inflammation and mucus production.
- Biologic Therapies: For severe asthma, biologics like omalizumab target specific molecules in the immune system to reduce inflammation.
2. Asthma Action Plan
Developing a personalized action plan with your healthcare provider is crucial. This plan should include:
- Daily Management: Details on daily medication use and monitoring.
- Recognizing Symptoms: How to identify worsening symptoms or early signs of an asthma attack.
- Steps to Take: Actions to manage symptoms and when to seek emergency care.
3. Trigger Avoidance
Identifying and avoiding triggers that can worsen symptoms is essential. Common triggers include:
- Allergens: Pollen, dust mites, pet dander, mold, and cockroach waste.
- Irritants: Tobacco smoke, air pollution, chemical fumes, and strong odors.
- Respiratory Infections: Colds, flu, and other respiratory infections.
- Weather Conditions: Cold air, changes in temperature, and humidity.
- Exercise: Particularly strenuous activity can trigger symptoms, known as exercise-induced bronchoconstriction (EIB).
- Emotions: Stress and strong emotions can also act as triggers.
4. Monitoring Your Condition
Regular monitoring of your asthma helps in keeping it under control:
- Peak Flow Meter: This device measures how well your lungs are working. Regular use can help detect early signs of worsening diseas.
- Symptom Diary: Keeping track of symptoms, triggers, and medication use can help identify patterns and improve management strategies.
5. Healthy Lifestyle
Adopting a healthy lifestyle can significantly improve asthma control:
- Regular Exercise: Physical activity can strengthen respiratory muscles, but it’s important to manage exercise-induced symptoms.
- Balanced Diet: A diet rich in fruits, vegetables, and whole grains can support overall health and reduce inflammation.
- Adequate Sleep: Good sleep hygiene can help reduce symptoms and improve overall well-being.
- Weight Management: Maintaining a healthy weight can reduce the severity of symptoms.
6. Education and Support
Educating yourself and those around you about asthma is vital:
- Asthma Education: Understanding your condition, medications, and management strategies empowers you to take control.
- Support Groups: Joining support groups can provide emotional support and practical tips from others living with asthma.
7. Emergency Preparedness
Being prepared for an asthma emergency can save lives:
- Know the Signs: Recognize the symptoms of a severe asthma attack, such as extreme breathlessness, inability to speak in full sentences, and blue lips or face.
- Action Plan: Follow the emergency steps outlined in your asthma action plan.
- Seek Help: Don’t hesitate to seek emergency medical attention if symptoms are severe and do not improve with quick-relief medications.
Recent Advancements in Treatment
Advancements in medical research have led to new treatments and improved management strategies. Some of the recent developments include:
- Biologic Therapies: Target specific pathways involved in the inflammatory process of asthma, providing relief for severe cases.
- Smart Inhalers: Devices that track medication usage and provide reminders, helping patients adhere to their treatment plans.
- Personalized Medicine: Tailoring treatment plans based on individual genetic and environmental factors for better outcomes.
How to stop asthma wheezing without inhaler ?
To stop asthma wheezing without an inhaler, you can:
- Sit Upright: Avoid lying down to help keep your airways open.
- Stay Calm: Anxiety can worsen wheezing, so try to remain calm.
- Deep Breathing: Take slow, deep breaths to help control breathing and open airways.
- Warm, Moist Air: Inhale steam from a warm shower or a bowl of hot water to help ease breathing.
- Drink Warm Fluids: Warm beverages can help relax the airways.
- Identify and Remove Triggers: Move away from any known triggers, such as smoke or allergens.
If symptoms persist or worsen, seek medical help immediately.
Conclusion
Asthma is a common yet complex condition that requires careful management and awareness. With the right treatment and lifestyle adjustments, asthmatic individuals can lead healthy and active lives. If you or someone you know is living with asthma, it is essential to work closely with healthcare providers to develop an effective management plan and stay informed about the latest advancements in treatment.
Is asthma genetic?
Yes, asthma has a genetic component. Family history of asthma and other allergic conditions increases the likelihood of developing asthma. Multiple genes are involved, affecting immune response and airway function, but environmental factors also play a significant role in its development and exacerbation.
Is there any association between asthma and allergy ?
Asthma is often associated with allergies. Allergens such as pollen, dust mites, mold, pet dander, and certain foods can trigger asthma symptoms. Many individuals with asthma also have allergic rhinitis (hay fever) or eczema, conditions that are part of the atopic or allergic triad, indicating a common underlying hypersensitivity in the immune system.
What are the Asthma self-care?
Self-care for asthma includes: Medication Adherence: Take prescribed medications as directed, including inhalers and any maintenance drugs. Avoid Triggers: Identify and avoid allergens or irritants that trigger asthma symptoms, such as pollen, dust mites, smoke, and strong odors. Regular Monitoring: Use a peak flow meter to monitor lung function and recognize early signs of an asthma attack. Asthma Action Plan: Follow a personalized asthma action plan developed with your healthcare provider. Healthy Lifestyle: Maintain a healthy diet, exercise regularly, and manage stress. Vaccinations: Stay up-to-date with flu and pneumonia vaccinations to prevent respiratory infections. Environmental Control: Keep the home clean, reduce dust, and use air filters to minimize exposure to allergens. Emergency Preparedness: Know when to seek medical help and keep rescue inhalers accessible.
What are the relation between Eosinophils and Asthma ?
Eosinophils are white blood cells involved in the immune response and inflammation. In asthma, elevated eosinophil levels can contribute to airway inflammation and hyperresponsiveness, leading to asthma symptoms. Eosinophilic asthma is a subtype characterized by high eosinophil counts, often requiring specific treatments like corticosteroids to reduce inflammation and manage symptoms.
is asthma a disability ?
Yes, asthma can be considered a disability if it significantly impairs a person's ability to perform daily activities or work. Under laws like the Americans with Disabilities Act (ADA), individuals with severe asthma that affects their quality of life and ability to function are entitled to reasonable accommodations and protections against discrimination.
Can you grow out of asthma?




