Hyperthyroidism, also known as an overactive thyroid, is a condition where the thyroid gland produces excessive amounts of thyroid hormones. These hormones, which include thyroxine (T4) and triiodothyronine (T3), regulate metabolism, heart rate, temperature, and other vital functions. When these hormones are in excess, they can accelerate the body’s metabolism, leading to a range of symptoms and health issues. In this blog, we’ll explore the causes, symptoms, diagnosis, and management of hyperthyroidism.
Causes of Hyperthyroidism
Hyperthyroidism, also known as overactive thyroid, occurs when the thyroid gland produces too much of the hormone thyroxine. This excess of thyroid hormones can accelerate the body’s metabolism, leading to a range of symptoms. The causes of hyperthyroidism are varied, involving autoimmune disorders, nodules, inflammation, excessive iodine intake, and certain medications. Here’s a closer look at each of these causes:
1. Graves’ Disease
- Autoimmune Disorder: Graves’ disease is the most common cause of hyperthyroidism. It is an autoimmune disorder where the immune system mistakenly attacks the thyroid gland, causing it to produce excessive thyroid hormones.
- TSI Antibodies: In Graves’ disease, the body produces thyroid-stimulating immunoglobulins (TSI) that mimic thyroid-stimulating hormone (TSH), leading to increased thyroid hormone production.
2. Thyroid Nodules
- Nodular Thyroid Disease: Hyperthyroidism can result from nodules or lumps in the thyroid gland. These nodules can become overactive and produce excessive thyroid hormones.
- Toxic Multinodular Goiter: This condition involves multiple overactive nodules within the thyroid gland.
- Solitary Toxic Adenoma: A single overactive nodule that produces excess thyroid hormones.

3. Thyroiditis
- Inflammation of the Thyroid: Thyroiditis refers to inflammation of the thyroid gland, which can cause stored thyroid hormone to leak into the bloodstream, leading to temporary hyperthyroidism.
- Subacute Thyroiditis: Often caused by a viral infection, it leads to painful inflammation and release of thyroid hormones.
- Silent Thyroiditis: A painless form of thyroiditis, often autoimmune in nature, that can also lead to temporary hyperthyroidism.
- Postpartum Thyroiditis: This can occur in some women after childbirth, causing temporary hyperthyroidism followed by hypothyroidism.
4. Excessive Iodine Intake
- Iodine and Thyroid Hormone Production: The thyroid gland uses iodine to produce thyroid hormones. Excessive iodine intake can lead to overproduction of these hormones.
- Sources of Excess Iodine: This can come from dietary sources, iodine supplements, or medications containing iodine, such as amiodarone (used to treat certain heart conditions) and certain contrast dyes used in imaging tests.
5. Medications
- Thyroid Hormone Medications: Overuse or incorrect dosage of thyroid hormone replacement therapy (e.g., levothyroxine) can cause hyperthyroidism.
- Amiodarone: A medication used to treat heart rhythm disorders that contains a high amount of iodine and can induce hyperthyroidism.
6. Other Causes
- Pituitary Adenoma: Rarely, a tumor in the pituitary gland can produce excessive TSH, stimulating the thyroid to produce more hormones.
- Struma Ovarii: A rare type of ovarian tumor that contains thyroid tissue, which can produce thyroid hormones and cause hyperthyroidism.
Symptoms of Hyperthyroidism
The symptoms of hyperthyroidism can vary and may develop gradually. Common symptoms include:
- Weight Loss: Despite an increased appetite, individuals may lose weight.
- Rapid Heartbeat: Palpitations or a racing heart are common.
- Increased Appetite: A noticeable increase in hunger.
- Nervousness or Anxiety: Feeling jittery, anxious, or irritable.
- Tremors: Slight shaking, usually in the hands and fingers.
- Sweating and Heat Intolerance: Excessive sweating and an inability to tolerate heat.
- Changes in Menstrual Patterns: Lighter, less frequent periods in women.
- Fatigue and Muscle Weakness: General tiredness and muscle weakness.
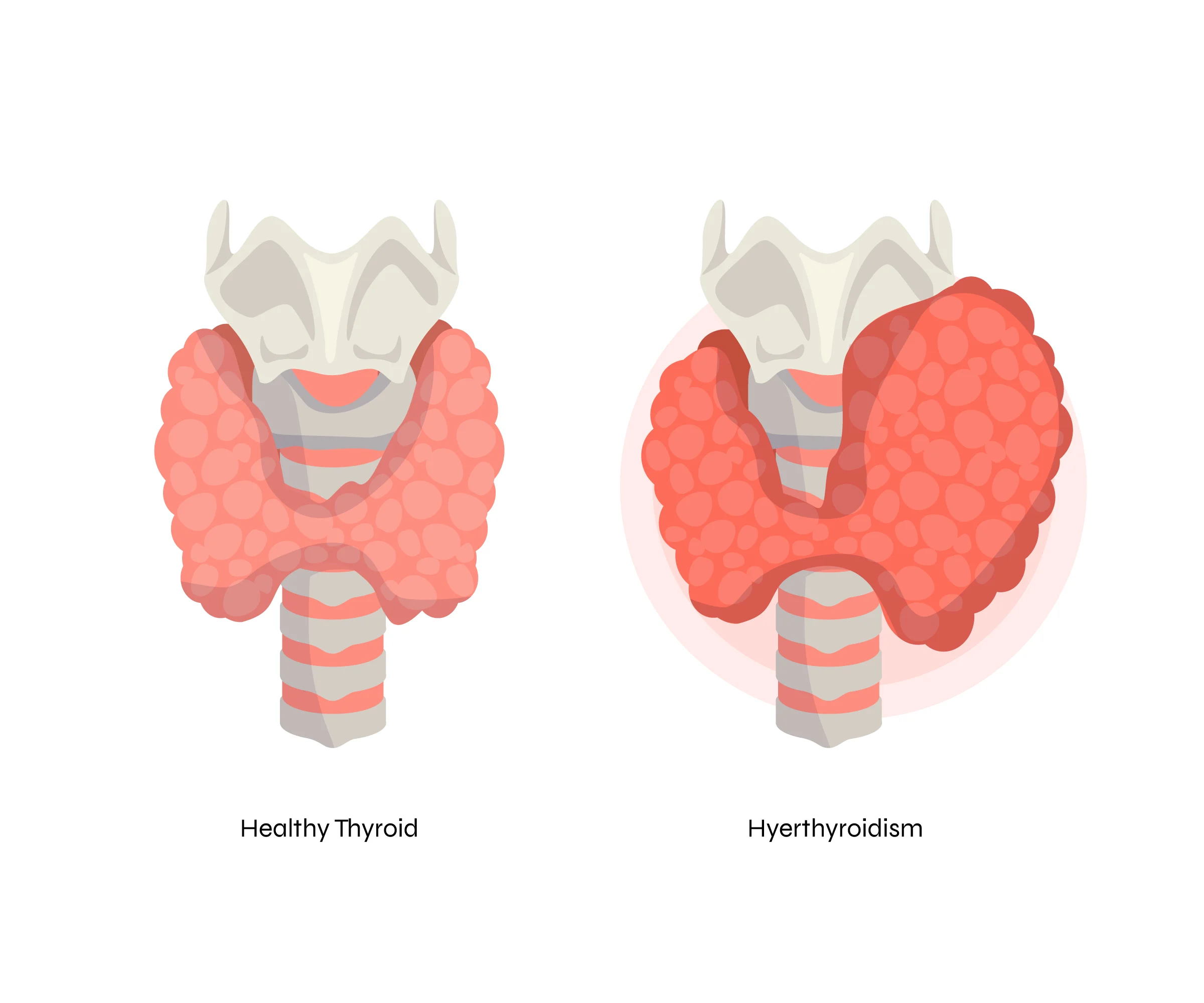
- Enlarged Thyroid Gland (Goiter): Swelling at the base of the neck.
- Sleep Disturbances: Difficulty sleeping or insomnia.
Diagnosis of Hyperthyroidism
This involves a thorough assessment that includes a detailed medical history, physical examination, and a series of laboratory and imaging tests. These steps help confirm the diagnosis, determine the severity of the condition, and identify the underlying cause. Here’s a comprehensive overview of the diagnostic process for hyperthyroidism:
1. Medical History
- Symptoms: The doctor will inquire about symptoms commonly associated with hyperthyroidism, such as weight loss, rapid heartbeat, increased appetite, nervousness, and tremors.
- Family History: Information about any family history of thyroid disease or autoimmune conditions.
- Medical History: Review of the patient’s overall health, including any previous thyroid problems, other medical conditions, medications, and recent procedures that could influence thyroid function.
2. Physical Examination
During a physical examination, the doctor will look for signs that suggest hyperthyroidism:
- Enlarged Thyroid Gland (Goiter): Swelling in the neck that indicates an enlarged thyroid gland.
- Eye Changes: Bulging eyes or other eye abnormalities associated with Graves’ disease.
- Skin and Hair: Changes such as thinning skin, fine or brittle hair, and excessive sweating.
- Heart Rate and Rhythm: Rapid heartbeat (tachycardia), irregular heartbeats (arrhythmias), or palpitations.
- Tremors: Slight shaking, particularly in the hands and fingers.
3. Laboratory Tests
Laboratory tests are essential for confirming hyperthyroidism and understanding its severity:
- Thyroid Function Tests
- Thyroid-Stimulating Hormone (TSH): Low levels of TSH typically indicate hyperthyroidism since the pituitary gland reduces TSH production in response to high thyroid hormone levels.
- Free Thyroxine (Free T4) and Triiodothyronine (Free T3): Elevated levels of these thyroid hormones confirm hyperthyroidism.
- Thyroid Antibodies
- Thyroid-Stimulating Immunoglobulin (TSI): Elevated in Graves’ disease, indicating an autoimmune cause.
- Anti-Thyroid Peroxidase (anti-TPO) and Anti-Thyroglobulin Antibodies: May be elevated in autoimmune thyroid diseases.
4. Imaging Tests
Imaging tests help visualize the thyroid gland and assess its activity:
- Radioactive Iodine Uptake Test
- Procedure: The patient ingests a small amount of radioactive iodine, and the thyroid’s uptake of the iodine is measured after a specified period.
- Purpose: Determines how much iodine the thyroid absorbs, helping to identify the cause of hyperthyroidism (e.g., Graves’ disease, thyroid nodules, thyroiditis).
- Thyroid Scan
- Procedure: After radioactive iodine or technetium is administered, a special camera creates an image of the thyroid.
- Purpose: Provides detailed information about the size, shape, and function of the thyroid gland, and identifies nodules or other abnormalities.
- Ultrasound
- Procedure: Uses sound waves to create images of the thyroid gland.
- Purpose: Detects nodules, goiter, and other structural abnormalities.
5. Additional Tests
In some cases, additional tests may be necessary to evaluate the overall health and rule out other conditions:
- Electrocardiogram (ECG): Assesses heart rhythm and detects any arrhythmias caused by hyperthyroidism.
- Blood Tests: Evaluate overall health, including liver function, kidney function, and blood glucose levels, as hyperthyroidism can affect multiple body systems.
Management of Hyperthyroidism
It involves a multifaceted approach tailored to the underlying cause, the severity of the condition, and the patient’s overall health. The primary goals of treatment are to reduce the excessive production of thyroid hormones, alleviate symptoms, and prevent complications. Here’s a comprehensive guide to the management of hyperthyroidism:
1. Medications
Anti-Thyroid Medications
- Methimazole: Inhibits the production of thyroid hormones. It is commonly used due to its efficacy and fewer side effects.
- Propylthiouracil (PTU): Also inhibits thyroid hormone production and is preferred during the first trimester of pregnancy due to its safety profile.
- Monitoring: Regular blood tests are required to monitor thyroid hormone levels and adjust the dosage accordingly.
Beta-Blockers
- Propranolol, Atenolol, Metoprolol: These medications do not lower thyroid hormone levels but help manage symptoms such as rapid heartbeat, palpitations, and tremors.
- Symptom Relief: Beta-blockers provide quick relief of hyperthyroid symptoms while waiting for anti-thyroid medications to take effect.
2. Radioactive Iodine Therapy
- Mechanism: Radioactive iodine is taken orally and absorbed by the thyroid gland, where it destroys overactive thyroid cells.
- Effectiveness: This treatment is effective in reducing thyroid hormone production and is a common choice for treating Graves’ disease and toxic nodular goiter.
- Hypothyroidism Risk: Most patients develop hypothyroidism after treatment, requiring lifelong thyroid hormone replacement therapy.
3. Surgery
- Partial or Total Removal: Surgery involves the removal of part or all of the thyroid gland.
- Indications: Recommended for patients who cannot tolerate medications or radioactive iodine therapy, those with large goiters causing compression symptoms, or those with suspected thyroid cancer.
- Post-Surgery: Patients usually need thyroid hormone replacement therapy for life if the entire gland is removed.
4. Lifestyle and Dietary Adjustments
Balanced Diet
- Nutrient-Rich Foods: Emphasize a diet rich in fruits, vegetables, whole grains, and lean proteins.
- Avoid Excessive Iodine: Limit intake of iodine-rich foods (e.g., seaweed, iodized salt) and supplements, as they can exacerbate hyperthyroidism.
Regular Exercise
- Moderate Activity: Engage in regular physical activity to maintain overall health and manage symptoms such as anxiety and restlessness.
- Strength Training: Incorporate strength training exercises to counteract muscle weakness.
Stress Management
- Relaxation Techniques: Practice stress-reducing activities such as yoga, meditation, and deep-breathing exercises to help manage anxiety and stress levels.
5. Regular Monitoring and Follow-Up
- Thyroid Function Tests: Regular blood tests to monitor thyroid hormone levels and adjust treatment as needed.
- Healthcare Provider Visits: Ongoing check-ups to assess the effectiveness of treatment and make necessary adjustments.
- Symptom Tracking: Keep a record of symptoms to discuss with your healthcare provider, ensuring optimal management.
6. Managing Underlying Conditions
- Graves’ Disease: Treat the autoimmune aspect with medications and possibly surgery if needed.
- Thyroiditis: Address the inflammation causing hormone leakage, which may involve anti-inflammatory medications or simply monitoring as the condition often resolves on its own.
7. Special Considerations
Pregnancy
- Monitoring and Adjustment: Pregnant women with hyperthyroidism require careful monitoring and adjustment of medications to avoid complications for both mother and baby.
- Safe Medications: PTU is preferred during the first trimester, switching to methimazole for the remainder of the pregnancy.
Elderly Patients
- Gentle Approach: Elderly patients may require a more cautious approach due to the higher risk of cardiovascular complications.
Can hyperthyroidism cause headaches?
Yes, hyperthyroidism can indeed cause headaches. Here’s how:
- Increased Metabolism: It accelerates the body’s metabolism, which can lead to physiological changes that trigger headaches.
- Blood Flow Changes: Thyroid hormones can affect blood flow regulation in the brain, potentially causing headaches.
- Eye Strain: Graves’ disease can lead to eye-related symptoms such as bulging eyes (exophthalmos) and eye irritation, which may contribute to headaches.
- Stress and Anxiety: Hyperthyroidism often causes symptoms like nervousness, irritability, and anxiety, which can also lead to tension headaches.
- Other Factors: Hormonal imbalances caused by hyperthyroidism can disrupt various bodily functions, potentially contributing to headache development.
If you are experiencing headaches along with other symptoms suggestive of hyperthyroidism (such as weight loss, palpitations, sweating, and tremors), it’s important to consult with a healthcare provider for proper evaluation and management.
Conclusion
Hyperthyroidism is a manageable condition with proper diagnosis and treatment. If you experience symptoms of hyperthyroidism, it’s essential to consult a healthcare provider for an accurate diagnosis and appropriate treatment plan. Early detection and management can help prevent complications and improve quality of life. By understanding the causes, recognizing the symptoms, and knowing the treatment options, individuals can take proactive steps to manage hyperthyroidism effectively.
FAQs,
What is hyperthyroidism?
It is a condition where the thyroid gland produces an excess of thyroid hormones, primarily thyroxine (T4) and triiodothyronine (T3), leading to an overactive metabolism.
What causes hyperthyroidism?
The most common cause is Graves' disease, an autoimmune disorder where the immune system mistakenly attacks the thyroid gland. Other causes include thyroid nodules (toxic adenomas), thyroiditis (inflammation of the thyroid gland), and excessive iodine intake.
What are the symptoms of hyperthyroidism?
Symptoms can vary but often include: Rapid heartbeat (tachycardia) Weight loss despite increased appetite Heat intolerance and excessive sweating Tremors, nervousness, and anxiety Fatigue or muscle weakness Difficulty sleeping Increased frequency of bowel movements
How is hyperthyroidism diagnosed?
Diagnosis typically involves: Physical examination to assess symptoms and signs like rapid heart rate and enlarged thyroid gland. Blood tests to measure levels of thyroid hormones (T4, T3) and thyroid-stimulating hormone (TSH). Radioactive iodine uptake (RAIU) test and thyroid scan to determine the cause of hyperthyroidism, especially if it's due to Graves' disease.
Can hyperthyroidism affect pregnancy?
Yes, untreated or poorly controlled hyperthyroidism during pregnancy can lead to complications such as preterm birth, low birth weight, preeclampsia (high blood pressure), and fetal thyroid dysfunction. It's crucial for pregnant women with hyperthyroidism to receive appropriate medical management.
What are the treatment options for hyperthyroidism?
Treatment depends on the underlying cause and severity but may include: Antithyroid medications (such as methimazole or propylthiouracil) to reduce thyroid hormone production. Radioactive iodine therapy (only used in non-pregnant adults) to destroy a portion of the thyroid gland. Surgery (thyroidectomy) to remove part or all of the thyroid gland, particularly for large goiters or when other treatments are not suitable.
What should I do if I suspect I have hyperthyroidism?
If you experience symptoms suggestive of hyperthyroidism, such as rapid heartbeat, unexplained weight loss, or excessive sweating, consult a healthcare provider. They can perform the necessary tests to diagnose hyperthyroidism and recommend appropriate treatment.
Can hyperthyroidism lead to other health problems?
Untreated hyperthyroidism can lead to serious complications such as heart problems (including atrial fibrillation), osteoporosis (bone thinning), and thyroid storm (a life-threatening condition with severe symptoms). Timely diagnosis and treatment can help prevent these complications.
Can hyperthyroidism be managed naturally or with dietary changes?
While dietary changes and complementary therapies may support overall health, they are not sufficient to treat hyperthyroidism alone. Medical treatment, under the guidance of a healthcare provider, is necessary to effectively manage hyperthyroidism and prevent complications.




