Understanding Hyperlipidemia: Causes, Symptoms, and Management
Hyperlipidemia, commonly known as high cholesterol, is a prevalent health condition characterized by elevated levels of lipids (fats) in the blood. These lipids primarily include cholesterol and triglycerides, essential substances for various bodily functions but harmful in excess. Hyperlipidemia is a significant risk factor for cardiovascular diseases, including heart attacks and strokes. This blog aims to provide a comprehensive understanding of hyperlipidemia, its causes, symptoms, and management strategies.
What is Hyperlipidemia?
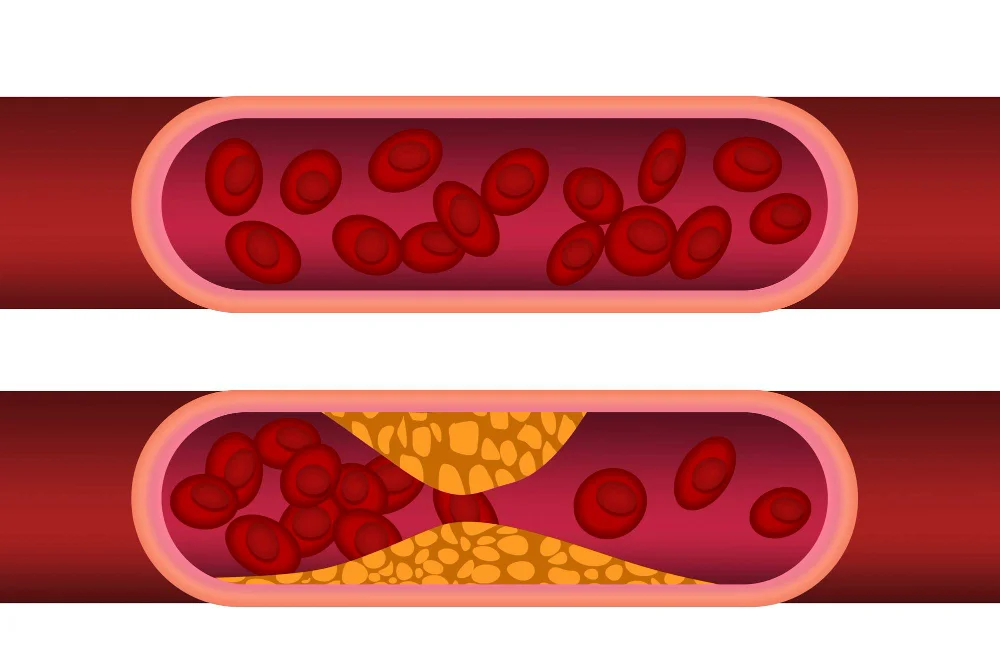
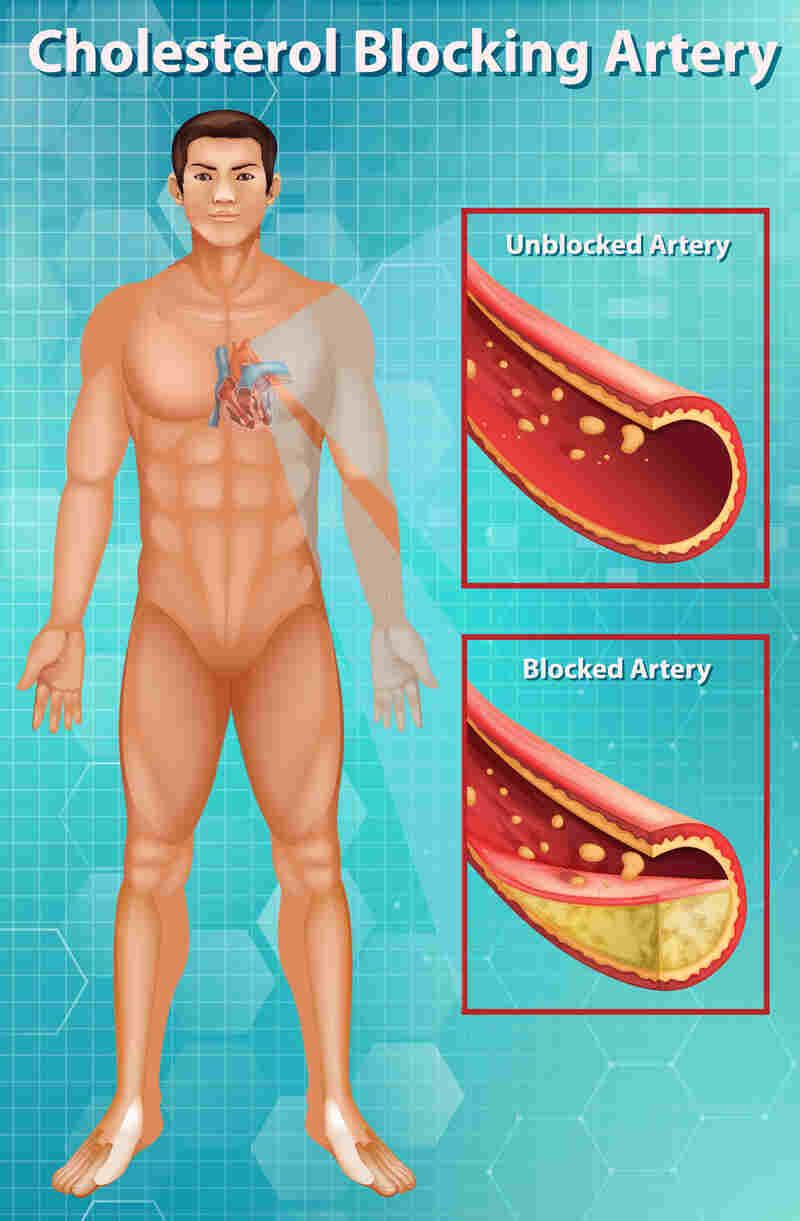
Hyperlipidemia refers to an abnormal increase in the levels of lipids in the blood. The condition is often diagnosed through lipid panel tests that measure total cholesterol, low-density lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL) cholesterol, and triglycerides. LDL cholesterol, often termed “bad” cholesterol, contributes to the buildup of fatty deposits in arteries, increasing the risk of heart disease. HDL cholesterol, or “good” cholesterol, helps remove LDL cholesterol from the bloodstream.
Causes of Hyperlipidemia
Hyperlipidemia, characterized by elevated levels of lipids (fats) in the blood, can result from various factors. Understanding these causes is crucial for effective prevention and management. Here are the primary contributors to hyperlipidemia:
1. Genetics
- Familial Hypercholesterolemia: A hereditary condition where individuals have significantly high cholesterol levels from a young age due to genetic mutations. This can lead to early-onset cardiovascular disease if not managed properly.
2. Diet
- High Saturated Fats: Consuming foods rich in saturated fats, such as red meat, full-fat dairy products, and fried foods, can raise LDL cholesterol levels.
- Trans Fats: Found in many processed foods, baked goods, and margarines, trans fats increase LDL cholesterol and lower HDL cholesterol, contributing to hyperlipidemia.
- Cholesterol-Rich Foods: While dietary cholesterol has a smaller impact on blood cholesterol for most people, excessive intake from sources like organ meats and shellfish can still be a contributing factor.
3. Lack of Physical Activity
- Sedentary Lifestyle: Physical inactivity can lead to weight gain, increased LDL cholesterol, and decreased HDL cholesterol. Regular exercise helps maintain a healthy weight and improves lipid profiles.
4. Obesity
- Excess Body Fat: Particularly visceral fat (fat around the abdomen) is associated with higher levels of LDL cholesterol and triglycerides. Obesity also contributes to insulin resistance, which can further worsen lipid levels.
5. Medical Conditions
- Diabetes: Poorly controlled diabetes can lead to higher triglyceride levels and lower HDL cholesterol.
- Hypothyroidism: Underactive thyroid can cause increased levels of total cholesterol and LDL cholesterol.
- Kidney Disease: Chronic kidney disease can disrupt lipid metabolism, leading to elevated cholesterol and triglyceride levels.
- Liver Disease: Conditions affecting the liver, such as nonalcoholic fatty liver disease (NAFLD), can also impact lipid levels.
6. Medications
- Certain Drugs: Some medications, including steroids, beta-blockers, diuretics, and antiretroviral drugs, can adversely affect lipid levels. It’s important to discuss potential side effects with your healthcare provider.
7. Lifestyle Factors
- Smoking: Smoking lowers HDL cholesterol and damages the blood vessels, making it easier for cholesterol to build up and form plaques.
- Excessive Alcohol Consumption: Drinking too much alcohol can raise triglyceride levels and contribute to liver damage, which affects lipid metabolism.
8. Age and Gender
- Age: As people age, their risk of hyperlipidemia increases. Post-menopausal women often see an increase in LDL cholesterol.
- Gender: Men typically have higher cholesterol levels than women until women reach menopause, after which their risk increases.
Symptoms and Signs of Hyperlipidemia
Hyperlipidemia itself often does not present noticeable symptoms until it progresses to more severe health complications. However, there are signs and symptoms associated with advanced stages of the condition and its complications.
Symptoms of Hyperlipidemia Complications
Symptoms are subjective experiences reported by the patient. In the case of hyperlipidemia, these are often related to complications from atherosclerosis:
- Chest Pain (Angina)
- Description: Discomfort or pain in the chest, often triggered by physical activity or stress.
- Cause: Reduced blood flow to the heart muscle.
- Shortness of Breath
- Description: Difficulty breathing or feeling winded, especially during physical exertion.
- Cause: Reduced oxygen supply to the heart and muscles.
- Pain in the Limbs
- Description: Cramping, aching, or pain in the legs or hips, particularly during walking or exercise (intermittent claudication).
- Cause: Reduced blood flow to the limbs due to peripheral artery disease (PAD).
- Fatigue
- Description: Persistent tiredness or lack of energy.
- Cause: Reduced oxygen and nutrient delivery to tissues due to narrowed arteries.
- Numbness or Weakness
- Description: Sudden numbness or weakness, especially on one side of the body.
- Cause: Stroke or transient ischemic attack (TIA), often due to reduced blood flow to the brain.
Signs of Hyperlipidemia Complications
Signs are objective findings observed by a healthcare provider during a physical examination or through diagnostic tests:
- Xanthomas
- Description: Yellowish, cholesterol-rich deposits under the skin, often on the elbows, knees, hands, feet, or around the eyes (xanthelasma).
- Cause: Elevated cholesterol levels, often associated with familial hypercholesterolemia.
- Arcus Senilis
- Description: A gray or white arc visible around the cornea of the eye.
- Cause: Lipid deposits in the cornea, commonly seen in older adults or those with very high cholesterol levels.
- Elevated Lipid Levels in Blood Tests
- Description: High levels of total cholesterol, LDL cholesterol, and triglycerides, with low levels of HDL cholesterol.
- Cause: Measured through lipid panel tests during routine check-ups.
- High Blood Pressure
- Description: Elevated blood pressure readings.
- Cause: Often associated with atherosclerosis and other cardiovascular conditions.
- Reduced Ankle-Brachial Index (ABI)
- Description: A lower ratio of the blood pressure in the ankle compared to the arm.
- Cause: Peripheral artery disease (PAD) due to atherosclerosis.
Importance of Monitoring
Due to the often asymptomatic nature of early-stage hyperlipidemia, regular screenings and check-ups are essential, particularly for individuals with risk factors like family history, obesity, diabetes, or hypertension. Early detection through blood tests and physical exams can help manage and mitigate the risk of severe complications.
Diagnosing Hyperlipidemia
Diagnosing hyperlipidemia involves a combination of medical history evaluation, physical examination, and laboratory tests. Early detection is crucial to prevent complications such as heart disease and stroke. Here’s a detailed overview of the diagnostic process:
1. Medical History
- Family History: A healthcare provider will inquire about any family history of hyperlipidemia or cardiovascular diseases, as genetic factors play a significant role.
- Personal History: Assessment of personal health history, including any existing medical conditions (e.g., diabetes, hypertension), lifestyle habits (diet, exercise, smoking, alcohol consumption), and use of medications that might affect lipid levels.
2. Physical Examination
During a physical examination, a healthcare provider might look for physical signs associated with hyperlipidemia and its complications:
- Xanthomas: Yellowish deposits of cholesterol under the skin, particularly around the eyes (xanthelasma) and on joints.
- Arcus Senilis: A gray or white arc visible around the cornea of the eye, often indicative of high cholesterol levels.
3. Laboratory Tests
The cornerstone of hyperlipidemia diagnosis is the lipid panel test, which measures the levels of different types of fats in the blood:
- Total Cholesterol: The overall amount of cholesterol in the blood. A level above 200 mg/dL is generally considered high.
- Low-Density Lipoprotein (LDL) Cholesterol: Often called “bad” cholesterol, high levels can lead to plaque buildup in arteries. Levels above 100 mg/dL may be concerning, especially in individuals with risk factors for heart disease.
- High-Density Lipoprotein (HDL) Cholesterol: Known as “good” cholesterol, it helps remove LDL cholesterol from the bloodstream. Levels below 40 mg/dL for men and 50 mg/dL for women are considered low.
- Triglycerides: A type of fat used for energy. Levels above 150 mg/dL are considered high.

4. Additional Tests
In some cases, additional tests may be conducted to assess the risk of cardiovascular diseases and to determine the underlying cause of hyperlipidemia:
- High-Sensitivity C-Reactive Protein (hs-CRP): Measures inflammation in the body, which can be a marker for heart disease.
- Lipoprotein(a): An inherited form of LDL cholesterol that can increase the risk of cardiovascular disease.
- Apolipoprotein B (ApoB): The main protein found in LDL cholesterol particles. High levels can indicate a higher risk of heart disease.
- Thyroid Function Tests: To rule out hypothyroidism as a contributing factor.
- Liver Function Tests: To check for liver diseases that can affect lipid levels.
5. Risk Assessment Tools
Healthcare providers often use risk assessment tools to evaluate the overall risk of cardiovascular disease. One commonly used tool is the Atherosclerotic Cardiovascular Disease (ASCVD) Risk Calculator, which considers factors like age, gender, race, blood pressure, cholesterol levels, smoking status, and diabetes.
Monitoring and Follow-Up
Regular monitoring is essential for individuals diagnosed with hyperlipidemia. Follow-up visits typically include:
- Periodic Lipid Panel Tests: To track the effectiveness of treatment and make necessary adjustments.
- Lifestyle and Medication Review: To ensure adherence to prescribed lifestyle changes and medications.
- Assessment of Cardiovascular Health: Ongoing evaluation of heart health and management of any other risk factors.
Management and Treatment
Managing hyperlipidemia involves a combination of lifestyle modifications, dietary changes, regular physical activity, and, when necessary, medication. The primary goal is to lower lipid levels, particularly low-density lipoprotein (LDL) cholesterol, to reduce the risk of cardiovascular disease. Here’s a comprehensive guide to managing hyperlipidemia:
1. Lifestyle Modifications
Dietary Changes
- Increase Fiber Intake: Incorporate more fruits, vegetables, whole grains, and legumes into your diet. Soluble fiber, found in foods like oats, beans, and certain fruits, can help lower LDL cholesterol.
- Choose Healthy Fats: Replace saturated fats (found in red meat and full-fat dairy products) with unsaturated fats (found in fish, nuts, seeds, and plant oils). Omega-3 fatty acids, found in fatty fish like salmon, are particularly beneficial.
- Limit Trans Fats: Avoid trans fats found in many processed and fried foods. Check food labels for partially hydrogenated oils.
- Reduce Dietary Cholesterol: Limit the intake of high-cholesterol foods such as organ meats and shellfish.
- Adopt a Heart-Healthy Diet: Consider diets like the Mediterranean diet, which emphasizes healthy fats, lean proteins, and plenty of fruits and vegetables, or the DASH diet, which is low in saturated fat, cholesterol, and total fat.
Regular Physical Activity
- Aerobic Exercise: Aim for at least 150 minutes of moderate-intensity aerobic exercise (such as brisk walking, cycling, or swimming) per week.
- Strength Training: Include muscle-strengthening activities at least two days per week.
- Consistency: Regular exercise can help raise HDL (good) cholesterol and lower LDL (bad) cholesterol and triglycerides.
Weight Management
- Achieve and Maintain a Healthy Weight: Losing excess weight can significantly improve lipid levels and reduce cardiovascular risk. Even a modest weight loss of 5-10% of body weight can make a difference.
Avoid Smoking
- Quit Smoking: Smoking lowers HDL cholesterol and increases the risk of heart disease. Quitting smoking can improve lipid levels and overall cardiovascular health.
Limit Alcohol Consumption
- Moderation: If you drink alcohol, do so in moderation. Excessive alcohol intake can raise triglyceride levels.
2. Medications
When lifestyle changes are insufficient to achieve desired lipid levels, medications may be prescribed. Common medications for managing hyperlipidemia include:
- Statins: These drugs are the most commonly prescribed for lowering LDL cholesterol. They work by inhibiting an enzyme involved in cholesterol production in the liver.
- Ezetimibe: This medication can help reduce the amount of cholesterol absorbed by the intestines.
- PCSK9 Inhibitors: These are newer drugs that can significantly lower LDL cholesterol by helping the liver absorb more LDL cholesterol.
- Bile Acid Sequestrants: These drugs help remove cholesterol from the bloodstream by binding to bile acids.
- Fibrates: Primarily used to lower triglycerides and, in some cases, increase HDL cholesterol.
- Niacin: Can help lower LDL cholesterol and triglycerides and raise HDL cholesterol, though it is less commonly used due to side effects.
- Omega-3 Fatty Acid Supplements: These can help lower triglycerides.
3. Regular Monitoring and Follow-Up
- Lipid Panel Tests: Regular blood tests to monitor cholesterol and triglyceride levels.
- Healthcare Provider Visits: Regular check-ups to assess the effectiveness of treatment and make any necessary adjustments.
- Cardiovascular Health Assessments: Ongoing evaluation of heart health, including blood pressure monitoring and screening for other risk factors.
4. Managing Underlying Conditions
- Control Diabetes: Proper management of blood sugar levels can help improve lipid profiles.
- Manage Hypertension: Controlling high blood pressure reduces the risk of cardiovascular complications associated with hyperlipidemia.
- Address Hypothyroidism: Treating an underactive thyroid can help normalize cholesterol levels.
Conclusion
Hyperlipidemia is a manageable condition with significant implications for cardiovascular health. Through a combination of lifestyle changes and medical interventions, individuals can effectively control their lipid levels and reduce their risk of serious complications. Regular check-ups and proactive management are crucial in maintaining heart health and overall well-being.
For personalized advice and treatment plans, consult with a healthcare provider. Taking proactive steps today can lead to a healthier tomorrow.
What is hyperlipidemia?
Hyperlipidemia is a condition characterized by elevated levels of lipids (fats) in the blood, including cholesterol and triglycerides. It increases the risk of cardiovascular diseases such as heart attacks and strokes.
What causes hyperlipidemia?
Hyperlipidemia can be caused by a combination of genetic, lifestyle, and medical factors, including a diet high in saturated and trans fats, lack of physical activity, obesity, diabetes, hypothyroidism, and certain medications.
What are the symptoms of hyperlipidemia?
Hyperlipidemia itself usually does not cause symptoms. However, it can lead to complications such as chest pain (angina), heart attack, stroke, and peripheral artery disease, which do present symptoms.
How is hyperlipidemia diagnosed?
Hyperlipidemia is diagnosed through blood tests that measure levels of total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides. A healthcare provider may also consider medical history, physical examination, and additional tests if necessary.
What are the risks associated with untreated hyperlipidemia?
Untreated hyperlipidemia can lead to the buildup of fatty deposits in the arteries (atherosclerosis), increasing the risk of heart attacks, strokes, and other cardiovascular diseases.
How can hyperlipidemia be managed?
Management involves lifestyle changes such as adopting a heart-healthy diet, regular physical activity, weight management, quitting smoking, and limiting alcohol consumption. Medications may also be prescribed to help lower lipid levels.
What dietary changes are recommended for managing hyperlipidemia?
A diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats is recommended. Reducing intake of saturated and trans fats, cholesterol, and refined sugars is essential. Foods high in soluble fiber and omega-3 fatty acids can help lower cholesterol levels.
What types of medications are used to treat hyperlipidemia?
Common medications include statins, ezetimibe, PCSK9 inhibitors, bile acid sequestrants, fibrates, niacin, and omega-3 fatty acid supplements. The choice of medication depends on the individual's specific lipid profile and overall health.
Can hyperlipidemia be prevented?
Preventing hyperlipidemia involves maintaining a healthy lifestyle, including a balanced diet, regular exercise, weight management, avoiding smoking, and limiting alcohol intake. Regular screening and early detection can also help prevent the condition.
How often should lipid levels be checked?
Lipid levels should be checked as part of regular health check-ups. Adults should have their lipid profiles checked every 4-6 years, or more frequently if they have risk factors for cardiovascular disease or are on treatment for hyperlipidemia.
Is hyperlipidemia hereditary?
Yes, hyperlipidemia can be hereditary. Familial hypercholesterolemia is a genetic condition that leads to high cholesterol levels from a young age and significantly increases the risk of cardiovascular disease.
What role does exercise play in managing hyperlipidemia?
Regular exercise helps improve lipid levels by raising HDL (good) cholesterol and lowering LDL (bad) cholesterol and triglycerides. It also aids in weight management and overall cardiovascular health.
What is the difference between LDL and HDL cholesterol?
Can children have hyperlipidemia?
Yes, children can have hyperlipidemia, especially if there is a family history of high cholesterol or cardiovascular diseases. Pediatricians may recommend screening and early intervention for children at risk.




