In the realm of cardiovascular health, one of the most prevalent and insidious conditions is atherosclerosis. Often described as the hardening or narrowing of arteries, atherosclerosis quietly progresses over many years, significantly increasing the risk of heart disease and stroke. Let’s delve into this complex yet crucial topic to grasp its impact on our health and the preventive measures we can take.
What is Atherosclerosis?
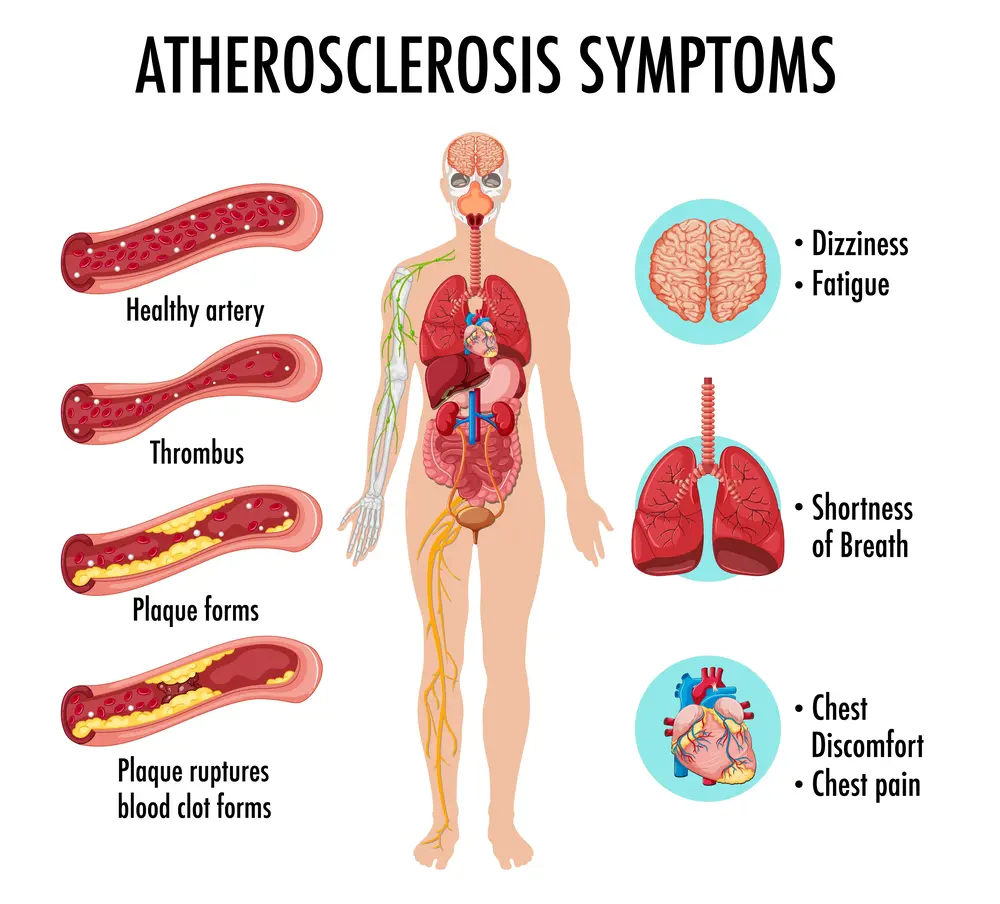
Atherosclerosis is a condition where fatty deposits, cholesterol, and other substances build up on the walls of arteries. Over time, these deposits form plaque, which can harden and narrow the arteries, restricting blood flow. This process can occur in arteries throughout the body, but it most commonly affects those supplying the heart (coronary arteries), brain (carotid arteries), and legs (peripheral arteries).
How Does Atherosclerosis Develop?
The development of atherosclerosis typically starts with damage to the inner layer of an artery. This damage can be caused by several factors, including:
- High blood pressure: Increased pressure can damage artery walls.
- High cholesterol: Elevated levels of LDL cholesterol (often termed “bad cholesterol”) can lead to plaque formation.
- Smoking: Chemicals in tobacco smoke can damage artery walls.
- Diabetes: High blood sugar levels can contribute to artery damage.
- Inflammation: Chronic inflammation can play a role in initiating and accelerating the process.
Once the artery wall is damaged, white blood cells move in to absorb cholesterol and other fats. Over time, these cells become engorged with cholesterol and can accumulate into fatty streaks, which eventually develop into larger plaques.
Consequences of Atherosclerosis
Atherosclerosis, the progressive buildup of plaque in arteries, has significant consequences for cardiovascular health and overall well-being. Here are some of the key consequences associated with atherosclerosis:
1. Coronary Artery Disease (CAD)
CAD occurs when atherosclerosis affects the arteries supplying blood to the heart muscle. The consequences can include:
- Angina: Chest pain or discomfort caused by reduced blood flow to the heart muscle.
- Heart Attack (Myocardial Infarction): Complete blockage of a coronary artery can lead to the death of heart muscle cells, resulting in a heart attack.
- Heart Failure: Over time, CAD can weaken the heart muscle, reducing its ability to pump effectively.
2. Carotid Artery Disease
Atherosclerosis in the carotid arteries, which supply blood to the brain, can lead to:
- Transient Ischemic Attacks (TIAs) or mini-strokes: Temporary episodes of neurological dysfunction due to temporary blockages in the brain’s blood supply.
- Stroke: A complete blockage or rupture of a plaque in the carotid artery can cause a stroke, resulting in permanent brain damage.
3. Peripheral Artery Disease (PAD)
PAD occurs when atherosclerosis affects arteries outside of the heart and brain, typically in the legs. Consequences include:
- Claudication: Pain or cramping in the legs during physical activity due to reduced blood flow.
- Critical Limb Ischemia: Severe PAD can lead to pain at rest, ulcers, or even gangrene, potentially requiring amputation.
4. Renal Artery Disease
Atherosclerosis affecting the renal arteries that supply blood to the kidneys can result in:
- Hypertension: Reduced blood flow to the kidneys can lead to high blood pressure.
- Kidney Failure: Severe narrowing or blockage of renal arteries can impair kidney function over time.
5. Aneurysms
Atherosclerosis can weaken arterial walls, increasing the risk of developing aneurysms (ballooning of the artery wall). Aneurysms can potentially rupture, causing life-threatening internal bleeding.
6. Risk of Blood Clots
Plaque in arteries can disrupt blood flow and promote the formation of blood clots. If a clot dislodges and travels to other parts of the body, it can block blood flow in critical arteries, leading to conditions such as pulmonary embolism (blockage in the lungs) or deep vein thrombosis.
7. Impact on Overall Cardiovascular Health
Atherosclerosis is not just a localized problem; it affects the entire cardiovascular system. Chronic inflammation and instability of plaques can lead to unpredictable complications like sudden cardiac death, even in individuals without prior symptoms.
Diagnosis
Diagnosing atherosclerosis typically involves a combination of assessing risk factors, conducting imaging tests, and sometimes performing procedures to evaluate the extent of arterial blockage and damage. Here’s an overview of the diagnostic process for atherosclerosis:
1. Clinical Evaluation and Risk Assessment
- Medical History: Your doctor will inquire about your medical history, including any symptoms (like chest pain or leg pain) and risk factors such as family history of heart disease, smoking habits, diet, and exercise patterns.
- Physical Examination: A physical exam may reveal signs such as weakened pulses in the legs or a bruit (abnormal sound) over an artery, which may suggest narrowing due to plaque buildup.
- Risk Factors: Evaluating risk factors such as high blood pressure, high cholesterol (especially LDL cholesterol), diabetes, obesity, and smoking is crucial as they contribute to the development and progression of atherosclerosis.
2. Diagnostic Tests
- Blood Tests: These may include lipid profile tests to measure cholesterol levels, including total cholesterol, LDL cholesterol (“bad” cholesterol), HDL cholesterol (“good” cholesterol), and triglycerides. Blood tests may also assess markers of inflammation and clotting factors.
- Electrocardiogram (ECG/EKG): This test records the electrical activity of the heart and can detect signs of previous heart attacks or abnormal heart rhythms.
- Stress Tests: These evaluate how your heart performs during physical activity and can help assess the presence of coronary artery disease (CAD).
- Imaging Tests:
- Echocardiogram: This ultrasound test uses sound waves to create images of the heart’s structure and function, helping to assess heart valves and blood flow.
- CT Scan (Computed Tomography) or MRI (Magnetic Resonance Imaging): These imaging tests can provide detailed pictures of the arteries and identify areas of plaque buildup.
- Angiography: Invasive angiography involves injecting a contrast dye into the arteries and using X-ray imaging to visualize the flow of blood through the arteries. It can pinpoint the location and severity of blockages caused by atherosclerosis.
- Carotid Ultrasound: This test uses sound waves to create images of the carotid arteries in the neck, assessing for plaque buildup and narrowing that could increase the risk of stroke.
3. Invasive Procedures
- Coronary Angiography: This procedure involves inserting a catheter into a blood vessel (usually in the groin or arm) and guiding it to the coronary arteries. Contrast dye is injected to visualize any blockages or narrowing in the arteries supplying the heart.
- Peripheral Angiography: Similar to coronary angiography, this procedure is used to examine arteries in the legs or other parts of the body affected by atherosclerosis.
4. Other Tests
- Ankle-Brachial Index (ABI): This test compares blood pressure in the ankle with blood pressure in the arm to assess peripheral artery disease (PAD).
Management
Managing atherosclerosis involves a combination of lifestyle modifications, medications, and in some cases, procedures to reduce the risk of complications and improve overall cardiovascular health. Here’s a comprehensive look at the strategies used in the management of atherosclerosis:
1. Lifestyle Modifications
Diet:
- Heart-Healthy Diet: Adopting a diet that is low in saturated fats, trans fats, and cholesterol can help manage cholesterol levels and reduce plaque buildup. Emphasize fruits, vegetables, whole grains, lean proteins (such as fish and poultry), and healthy fats (like olive oil and nuts).
- Limit Sodium: Lowering sodium intake helps manage blood pressure, reducing strain on the heart and arteries.
Exercise:
- Regular Physical Activity: Engaging in moderate-intensity aerobic exercise, such as brisk walking, swimming, or cycling, for at least 150 minutes per week can improve cardiovascular fitness and lower cholesterol levels.
Smoking Cessation:
- Quit Smoking: Smoking damages the walls of arteries and accelerates the progression of atherosclerosis. Quitting smoking reduces cardiovascular risk significantly.
Weight Management:
- Maintain a Healthy Weight: Losing excess weight and maintaining a healthy body weight can reduce strain on the heart and improve overall cardiovascular health.
2. Medications
Cholesterol-Lowering Medications:
- Statins: These drugs lower LDL cholesterol levels and have been shown to reduce the risk of heart attacks and strokes in people with atherosclerosis.
- Ezetimibe and PCSK9 Inhibitors: These medications may be prescribed in addition to statins or for individuals who cannot tolerate statins.
Blood Pressure Medications:
- ACE Inhibitors, ARBs, Beta-Blockers, Calcium Channel Blockers: These medications help manage high blood pressure, reducing the risk of complications from atherosclerosis.
Antiplatelet Medications:
- Aspirin or Clopidogrel: These medications help prevent blood clots from forming in narrowed arteries and reduce the risk of heart attack or stroke.
Other Medications:
- Diabetes Medications: If you have diabetes, managing blood sugar levels is crucial to prevent further damage to blood vessels.
3. Procedures and Surgery
Angioplasty and Stenting:
- Balloon Angioplasty: In this procedure, a small balloon is inflated inside a narrowed artery to widen it and improve blood flow.
- Stenting: A mesh tube (stent) may be placed in the artery during angioplasty to help keep it open.
Coronary Artery Bypass Grafting (CABG):
- Surgery: In severe cases of coronary artery disease, bypass surgery may be necessary to create new routes for blood flow to the heart muscle, bypassing blocked or narrowed arteries.
4. Cardiac Rehabilitation
- Structured Program: After a heart attack, heart surgery, or diagnosis of atherosclerosis, cardiac rehabilitation programs offer supervised exercise training, education on heart-healthy living, and support to improve cardiovascular health and reduce the risk of future heart problems.
5. Regular Medical Monitoring
- Follow-Up Visits: Regular visits to your healthcare provider are essential to monitor progress, adjust medications, and address any new symptoms or concerns.
The Importance Of Prevention
Preventing atherosclerosis involves adopting a healthy lifestyle and managing risk factors that contribute to the development and progression of this condition. Here are key strategies for preventing atherosclerosis:
1. Healthy Diet
- Eat Heart-Healthy Foods: Emphasize a diet rich in fruits, vegetables, whole grains, lean proteins (such as fish and poultry), and healthy fats (like olive oil and nuts).
- Limit Saturated and Trans Fats: Reduce intake of saturated fats found in red meat and full-fat dairy products, as well as trans fats found in processed and fried foods.
- Control Portions: Be mindful of portion sizes to maintain a healthy weight and avoid overeating, which can contribute to obesity and high cholesterol levels.
2. Regular Physical Activity
- Engage in Regular Exercise: Aim for at least 150 minutes of moderate-intensity aerobic activity (such as brisk walking, swimming, or cycling) per week, along with muscle-strengthening activities on two or more days per week.
- Stay Active Throughout the Day: Incorporate movement into your daily routine, such as taking stairs instead of elevators and parking farther away from destinations.
3. Quit Smoking
- Stop Smoking: Smoking damages the lining of blood vessels, promotes the buildup of plaque, and increases the risk of blood clots. Quitting smoking significantly reduces cardiovascular risk.
4. Manage Blood Pressure
- Monitor Blood Pressure: Have your blood pressure checked regularly and work with your healthcare provider to maintain healthy levels (typically below 120/80 mm Hg).
- Medication if Needed: If you have high blood pressure, follow your doctor’s recommendations for medications and lifestyle changes to control it effectively.
5. Manage Cholesterol Levels
- Monitor Cholesterol: Regularly check your cholesterol levels, including total cholesterol, LDL cholesterol (“bad” cholesterol), HDL cholesterol (“good” cholesterol), and triglycerides.
- Medication if Needed: If cholesterol levels are high, your doctor may prescribe medications such as statins to lower LDL cholesterol and reduce the risk of plaque buildup.
6. Control Diabetes
- Manage Blood Sugar: If you have diabetes, work with your healthcare team to keep blood sugar levels within target range to prevent damage to blood vessels.
- Healthy Lifestyle: Maintain a healthy diet, engage in regular physical activity, and take medications as prescribed to manage diabetes effectively.
7. Maintain a Healthy Weight
- Healthy BMI: Aim for a body mass index (BMI) within the healthy range (18.5 to 24.9) by adopting a balanced diet and staying physically active.
8. Reduce Stress
- Manage Stress: Practice stress-reduction techniques such as meditation, yoga, deep breathing exercises, or engaging in hobbies to lower stress levels, which can impact cardiovascular health.
9. Limit Alcohol Intake
- Moderate Consumption: If you drink alcohol, do so in moderation. Limit intake to no more than one drink per day for women and up to two drinks per day for men.
10. Regular Health Check-Ups
- Annual Check-Ups: Schedule regular visits with your healthcare provider for preventive care, screenings, and to monitor your cardiovascular health.
Conclusion
Atherosclerosis may be a silent condition, but its impact on cardiovascular health is profound. By understanding its development, consequences, and management strategies, we empower ourselves to take proactive steps towards heart health. With a combination of healthy living and medical guidance, we can mitigate the risks posed by atherosclerosis and strive towards a longer, healthier life.
Remember, a heart-healthy lifestyle is not just about preventing atherosclerosis but also about nurturing overall well-being. Stay informed, stay proactive, and prioritize your heart health—it’s the heartbeat of a fulfilling life.



