Introduction :
Chronic Obstructive Pulmonary Disease (COPD), is a progressive and debilitating respiratory disorder that affects millions of individuals worldwide. It is estimated to affect 32 million persons in the United States and is the third leading cause of death in the United States.
Chronic obstructive pulmonary disease (COPD) is a persistent inflammatory lung ailment characterized by restricted airflow from the lungs, leading to symptoms such as difficulty breathing, coughing, the production of mucus (sputum), and wheezing. The primary causative factor is typically prolonged exposure to irritants like noxious gases or particulate matter, with cigarette smoke being the most common source. Individuals afflicted with COPD face an elevated risk of developing additional health issues, including heart disease, lung cancer, and various other conditions.
Forms of COPD :
There are two main forms of COPD:
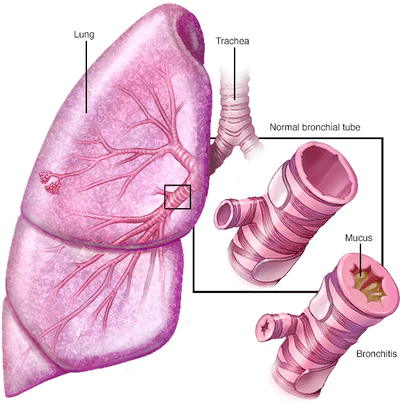
- Chronic bronchitis ,
In this health condition, the bronchial tubes undergo inflammation and constriction, leading to increased mucus production in the lungs. This excess mucus can exacerbate the blockage in the narrowed tubes. A persistent cough ensues as an attempt to clear the airways and alleviate the restricted breathing.
-
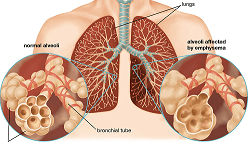
Emphysema,
Emphysema is a lung condition characterized by damage to the air sacs (alveoli) in the lungs. In emphysema, the walls of the alveoli become weak and lose their elasticity, leading to the destruction of the alveolar walls. This reduces the surface area available for gas exchange, resulting in difficulty in breathing.
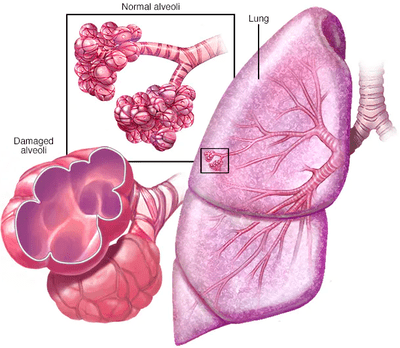
Many individuals diagnosed with COPD often experience a combination of both chronic bronchitis and emphysema. Despite being a progressive condition with a tendency to worsen over time, COPD is manageable. Through effective management, individuals with COPD can attain significant control over symptoms, leading to an improved quality of life and a decreased risk of associated conditions.
.
Causes :
Chronic Obstructive Pulmonary Disease is primarily caused by long-term exposure to irritants that damage the lungs and airways. The most common causes of COPD include:
- Cigarette Smoke: Smoking is the leading cause of Chronic Obstructive Pulmonary Disease . The harmful chemicals in tobacco smoke irritate the airways and lungs, leading to inflammation, narrowing of the air passages, and destruction of lung tissue over time. Even secondhand smoke can contribute to COPD development.
- Air Pollution: Exposure to indoor and outdoor air pollution, including fumes from burning fuels (such as wood or coal), industrial emissions, vehicle exhaust, and other pollutants, can increase the risk of developing Chronic Obstructive Pulmonary Disease . Indoor air pollutants like cooking fumes, chemicals, and dust in poorly ventilated spaces can also contribute.
- Occupational Exposure: Long-term exposure to dust, chemicals, and fumes in certain occupational settings can damage the lungs and contribute to COPD development. Industries such as mining, construction, manufacturing, agriculture, and firefighting pose higher risks for Chronic Obstructive Pulmonary Disease due to exposure to hazardous substances.
- Genetic Factors: Although less common, genetic factors can predispose individuals to Chronic Obstructive Pulmonary Disease . Alpha-1 antitrypsin deficiency is a genetic condition that can lead to early-onset COPD, particularly in individuals who have never smoked. This condition results in a deficiency of a protein that protects the lungs from damage.
- Indoor Biomass Fuel Use: In many developing countries, indoor cooking using biomass fuels such as wood, animal dung, or crop residues produces high levels of indoor air pollution. Prolonged exposure to these pollutants, especially in poorly ventilated homes, can increase the risk of Chronic Obstructive Pulmonary Disease.
- Respiratory Infections: Severe or recurrent respiratory infections, particularly during childhood, can cause lung damage and increase the risk of developing COPD later in life. Infections such as pneumonia and bronchitis, especially if left untreated or if the individual has underlying lung conditions, can contribute to COPD development.
- Aging: While not a direct cause, aging is a risk factor for Chronic Obstructive Pulmonary Disease . As individuals age, their lungs may naturally lose some elasticity and function. Combined with other risk factors such as smoking or environmental exposures, aging can exacerbate the development and progression of COPD.
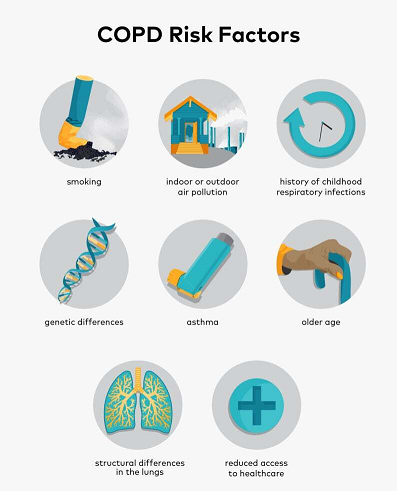
Risk Factor :
Chronic Obstructive Pulmonary Disease is often referred to as a “smoker’s disease” however although smoking is one of the main risk factors for developing COPD, people who never smoke may also develop COPD. Other risk factors may include:
A history of childhood respiratory infections
- Exposure to smoke from coal or wood-burning stoves
- Exposure to secondhand smoke
- People with a history of asthma
- People who have underdeveloped lungs
- Individuals aged 40 and older (as lung function tends to decline with age) are identified as causes and risk factors associated with COPD
However, it’s noteworthy that individuals residing in poverty and rural areas face an elevated likelihood of developing COPD. Beyond smoking status, some reasons for the increased risk may include exposures to indoor and outdoor pollutants, occupational exposures and lack of access to healthcare.
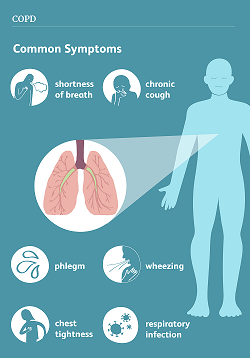
Symptoms :
Chronic Obstructive Pulmonary Disease symptoms often don’t appear until significant lung damage has occurred, and they usually worsen over time, particularly if smoking exposure continues.
The symptoms of COPD frequently remain latent until substantial lung damage has transpired, and they typically deteriorate gradually, especially in cases of persistent exposure to smoking.
Signs and symptoms of COPD may include:
- Shortness of breath, especially during physical activities
- Wheezing
- Chest tightness
- A persistent cough capable of producing mucus (sputum), which can vary in color from clear to white, yellow, or greenish.
- Frequent respiratory infections
- Lack of energy
- Unintended weight loss (in later stages)
- Swelling in ankles, feet or legs.
Individuals with COPD are prone to encountering episodes known as exacerbations, characterized by a worsening of symptoms beyond the typical day-to-day variations that persists for at least several days.
It is important to consult with your healthcare provider if your symptoms do not show improvement with treatment, worsen, or if you observe signs of infection, such as fever or changes in sputum.
Seek prompt medical attention if you find it difficult to breathe, experience severe blueness of the lips or fingernail beds (cyanosis), have a rapid heartbeat, or feel mentally foggy with difficulty concentrating
Diagnosis :
To diagnose Chronic Obstructive Pulmonary Disease , encompassing both chronic bronchitis and emphysema, your healthcare provider will assess your symptoms, inquire about your comprehensive health history, perform a physical examination, and analyze test results.
Following the initial visit, your provider will assess the severity of your condition and establish a personalized treatment plan. Subsequent follow-up visits will involve discussions between you and your healthcare provider regarding symptoms, the risk of COPD flare-ups or exacerbations, and adjustments to the treatment plan as necessary
History of Chronic Obstructive Pulmonary Disease ;
- When there is suspicion of COPD, your healthcare provider will gather a comprehensive health history and perform a physical examination. The medical history will likely include:
- Current or past smoking habits.
- Exposure to secondhand smoke, air pollution, previous work involving chemicals, dust, or fumes, and a history of childhood respiratory infections.
- Incidents of exacerbations or flare-ups, including any hospitalizations.
- Presence of symptoms such as shortness of breath, chronic cough, or the production of mucus (sputum or phlegm).
- Family history, particularly if any family members have been diagnosed with COPD, alpha-1 deficiency, or another chronic lung disease.
- Evaluation of how symptoms have impacted your daily life, including changes in activities or missed work.
- Identification of times when symptoms worsen, such as during a change of season, specific weather conditions, or exposure to triggers.
- Exploration of other comorbidities like heart disease, osteoporosis, anxiety, or depression.
This thorough assessment helps your healthcare provider in making an accurate diagnosis and developing an appropriate treatment plan
.
-
Testing for COPD ;
Your healthcare provider may conduct breathing tests or lung function tests as part of the diagnostic process.. These breathing tests can be done in your provider’s office while other tests may be done in a pulmonary function testing lab.
- Spirometry ;
- A spirometry test can diagnose COPD. These tests assist your healthcare provider in assessing the functionality of your lungs and determining how effectively they are working.
-
Alpha 1 antitrypsin ;
- Your healthcare provider may order a screening blood test to check the level of alpha-1 antitrypsin in your body.
-
Chest X-ray ;
- While a chest X-ray alone cannot conclusively diagnose COPD, it can serve to rule out other conditions with similar symptoms. Additionally, changes in the lungs associated with COPD may be visible on chest X-rays.
-
HRCT ;
- A HRCT may show the type of COPD like emphysema or chronic bronchitis, progression of the disease or severity.
-
Arterial blood gases or oximetry ;
- Oximetry or ABG measures the oxygen level in your blood.
-
Lung volume test ;
- It is to measure the volume of air in the lungs including the air that remains at the end of a normal breath
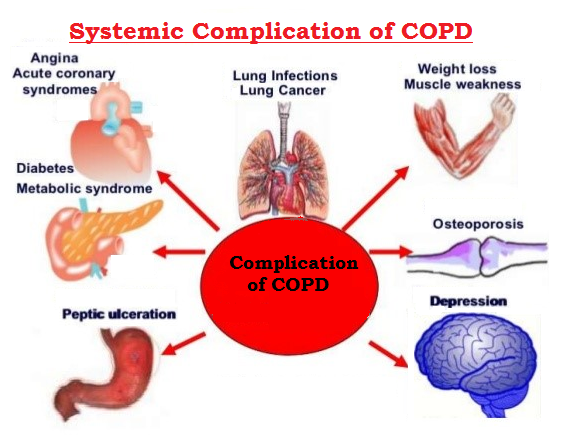
Complications :
Chronic Obstructive Pulmonary Disease can cause many complications, including:
- Respiratory infections. People with COPD are more likely to catch colds, the flu and pneumonia. Any respiratory infection has the potential to exacerbate breathing difficulties and may lead to additional damage to lung tissue.
- Heart problems. For reasons that aren’t fully understood, COPD can increase your risk of heart disease, including heart attack
- Lung cancer. Individuals with COPD face an elevated risk of developing lung cancer..
- High blood pressure in lung arteries. COPD can lead to high blood pressure in the arteries that supply blood to the lungs, a condition known as pulmonary hypertension..
- Depression. the challenges associated with difficulty breathing can impede engagement in enjoyable activities, contributing to the development of depression in individuals dealing with the serious illness of COPD .
Treatment :
Managing Chronic Obstructive Pulmonary Disease treatment guidelines involves a comprehensive approach aimed at relieving symptoms, improving lung function, preventing exacerbations, and enhancing overall quality of life. Here are key aspects of COPD management:
- Lifestyle Modifications:
- Smoking Cessation: The most important step in managing COPD is quitting smoking. Smoking cessation can slow the progression of the disease and improve symptoms.
- Avoiding Lung Irritants: Minimize exposure to indoor and outdoor air pollutants, such as dust, chemicals, fumes, and secondhand smoke. Proper ventilation in living spaces is essential.
- Regular Physical Activity: Engaging in regular exercise, such as walking or cycling, can improve muscle strength and endurance, reduce shortness of breath, and enhance overall fitness.
- Medications:
- Bronchodilators: These medications help relax the muscles around the airways, making it easier to breathe. They are often delivered through inhalers and can be short-acting (e.g., albuterol) for immediate relief or long-acting (e.g., tiotropium, salmeterol) for maintenance therapy.
- Inhaled Corticosteroids: These medications reduce airway inflammation and may be prescribed for individuals with frequent exacerbations or more severe COPD.
- Combination Therapy: Some medications combine bronchodilators with corticosteroids to provide both bronchodilation and anti-inflammatory effects.
- Phosphodiesterase-4 Inhibitors: These medications may be used in some cases to reduce inflammation and relax the airways, particularly in individuals with severe COPD and chronic bronchitis.
- Antibiotics and Antivirals: These may be prescribed during exacerbations of COPD to treat bacterial or viral infections.
- Pulmonary Rehabilitation:
- Exercise Training: Supervised exercise programs can help improve exercise tolerance, muscle strength, and overall quality of life.
- Education and Support: Pulmonary rehabilitation programs provide education on COPD management, breathing techniques, nutrition, and psychological support to cope with the emotional impact of the disease.
- Oxygen Therapy:
- Supplemental oxygen therapy may be prescribed for individuals with severe COPD and low blood oxygen levels, especially during physical activity and sleep, to improve oxygenation and reduce symptoms.
- Vaccinations:
- Annual influenza (flu) vaccination and periodic pneumococcal vaccination are recommended to reduce the risk of respiratory infections, which can exacerbate COPD symptoms.
- Management of Exacerbations:
- Early recognition and prompt treatment of exacerbations are essential to prevent further lung damage. Treatment may include bronchodilators, corticosteroids, antibiotics (if bacterial infection is present), and oxygen therapy.
- Developing a written action plan with healthcare providers can help individuals and caregivers know when to seek medical attention during exacerbations.
- Surgical Interventions:
- In severe cases of Chronic Obstructive Pulmonary Disease , surgical options such as lung volume reduction surgery (LVRS) or lung transplantation may be considered to improve lung function and quality of life.
Prevention ;
Chronic Obstructive Pulmonary Disease is a serious disease, but it is manageable. If you have COPD, it is important to work with your doctor to develop a treatment plan that is right for you. With proper treatment, you can live a long and active life.
Here are some additional tips for managing C.O.P.D:
Quit smoking.
This is the single most important thing you can do to improve your C.O.P.D symptoms.
Get regular exercise.
Eat a healthy diet.
Stay hydrated.
Ensuring adequate fluid intake can assist in thinning mucus, making it easier to expel through coughing.
Manage stress.
Occupational exposure
Frequently Asked Questions (FAQs) ;
What is COPD?
COPD stands for Chronic Obstructive Pulmonary Disease. It's a progressive lung disease that makes it hard to breathe. The term encompasses chronic bronchitis and emphysema, and it's often caused by long-term exposure to irritating gases or particulate matter, most commonly from cigarette smoke.
What are the common symptoms of COPD?
Common symptoms include shortness of breath, chronic cough, wheezing, and chest tightness. Individuals with Chronic Obstructive Pulmonary Disease may also experience exacerbations, characterized by a sudden worsening of symptoms.
What are the risk factors for COPD?
Smoking tobacco is the leading cause of COPD. Other risk factors include long-term exposure to lung irritants such as air pollution, chemical fumes, and dust. Genetics may also play a role.
How is Chronic Obstructive Pulmonary Disease diagnosed?
Diagnosis often involves a combination of medical history, physical examination, lung function tests (spirometry), and imaging studies such as chest X-rays or CT scans.
What are the treatment options for COPD?
Treatment aims to relieve symptoms, improve quality of life, and slow disease progression. Common treatments include bronchodilators (inhaled medications that help open airways), corticosteroids, pulmonary rehabilitation programs, supplemental oxygen therapy, and, in severe cases, surgical interventions such as lung volume reduction surgery or lung transplantation.
Can you prevent COPD from progressing
While COPD can't always be prevented, avoiding exposure to lung irritants such as tobacco smoke, air pollution, and occupational dust and chemicals can reduce the risk. Quitting smoking is the single most effective way to prevent COPD and slow its progression in those already diagnosed.
What lifestyle changes are recommended for COPD?
Lifestyle changes such as regular exercise, maintaining a healthy diet, staying hydrated, avoiding respiratory infections, and participating in pulmonary rehabilitation programs can help manage COPD symptoms and improve overall well-being.
COPD is a progressive disease, meaning it typically worsens over time. However, early diagnosis, appropriate treatment, and lifestyle modifications can help manage symptoms, improve quality of life, and slow disease progression.
What organizations help people with COPD?
Yes, many organizations and online communities exist for individuals with COPD and their caregivers. These groups can provide valuable information, resources, and emotional support for managing the challenges of living with COPD.
When should I see a doctor if I suspect I have COPD?
If you experience persistent respiratory symptoms such as shortness of breath, chronic cough, wheezing, or chest tightness, it's important to see a doctor for evaluation and diagnosis. Early detection and treatment can help slow the progression of the disease and improve outcomes.