Angioedema is a medical condition characterized by sudden swelling beneath the skin or mucous membranes. It commonly affects the face, lips, tongue, throat, and sometimes the extremities. The swelling is often due to an allergic reaction, but it can also have non-allergic causes.
What is Angioedema?
Angioedema involves the rapid swelling of the deeper layers of the skin and tissues just under the skin or mucous membranes. It shares some similarities with hives (urticaria), but while hives affect the surface of the skin, angioedema affects deeper layers.
Causes of Angioedema
Angioedema can be triggered by various factors, which can be broadly categorized into allergic and non-allergic causes. Understanding these causes is essential for effective management and prevention.
1. Allergic Angioedema
Allergic reactions are a common cause of angioedema, often involving the immune system’s response to certain allergens. Common allergens include:
- Foods: Certain foods are well-known triggers for allergic reactions that can lead to angioedema. These include:
- Nuts (e.g., peanuts, almonds)
- Shellfish (e.g., shrimp, crab)
- Eggs
- Dairy products
- Wheat
- Medications: Some medications can trigger allergic reactions. Common culprits include:
- Antibiotics (e.g., penicillin)
- Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and aspirin
- Insect Stings or Bites: Venom from insect stings or bites, particularly from bees, wasps, and ants, can cause severe allergic reactions.
- Latex: Latex products, such as gloves or balloons, can trigger allergic reactions in sensitive individuals.
2. Non-Allergic Angioedema
Non-allergic angioedema can be triggered by various factors unrelated to an allergic response. These include:
- Hereditary Angioedema (HAE): This rare genetic disorder affects blood proteins involved in inflammation. It is caused by a deficiency or dysfunction of C1 esterase inhibitor, a protein that helps regulate the immune system. HAE is often characterized by recurrent episodes of severe swelling.
- Medication-Induced: Certain medications, particularly angiotensin-converting enzyme (ACE) inhibitors used for hypertension, can be a causative agents. This type typically occurs within the first week of medication use but can develop even after prolonged use.
- Idiopathic Angioedema: In many cases, the cause of angioedema remains unknown. This is referred to as idiopathic angioedema. It can be challenging to identify triggers in these cases, making management more difficult.
- Physical Factors: Certain physical factors can sometimes trigger angioedema, including:
- Stress: Emotional stress can trigger in some individuals.
- Trauma: Physical trauma or injury to the skin can cause localized form.
- Infections: Bacterial, viral, or fungal infections can sometimes lead to angioedema as part of the body’s inflammatory response.
3. Other Causes
Additional factors that can contribute to the development of angioedema include:
- Hormonal Changes: Hormonal fluctuations, such as those occurring during menstruation, pregnancy, or hormone replacement therapy, can trigger in some individuals.
- Environmental Factors: Exposure to extreme temperatures, sunlight, or other environmental factors can sometimes precipitate allergic reaction.
Food To Avoid in Angioedema
- Histamine-Rich Foods:
- Aged cheeses
- Processed meats (e.g., salami, pepperoni)
- Fermented foods (e.g., sauerkraut, soy sauce)
- Alcoholic beverages (especially red wine and beer)
- Histamine-Releasing Foods:
- Strawberries
- Tomatoes
- Shellfish
- Nuts
- Chocolate
- Food Additives:
- Artificial colors (e.g., tartrazine)
- Preservatives (e.g., sulfites, benzoates)
- Flavor enhancers (e.g., monosodium glutamate (MSG))
- Common Allergens:
- Peanuts
- Tree nuts
- Fish
- Shellfish
- Eggs
- Milk
- Soy
- Wheat
For personalized advice, consult a healthcare professional.
Symptoms
The symptoms can vary in severity and may include:
- Swelling of the face, lips, tongue, throat, hands, or feet
- Red, raised areas on the skin (similar to hives)
- Pain or warmth in the affected areas
- Difficulty breathing or swallowing (in severe cases)
Diagnosis
It involves a comprehensive approach that includes a detailed medical history, physical examination, and various tests to identify the underlying cause. Proper diagnosis is crucial for effective treatment and management of the condition.
1. Medical History
The first step is taking a thorough medical history. The healthcare provider will ask about:
- Symptoms: Description of the swelling, including its location, duration, and severity.
- Triggers: Potential triggers such as foods, medications, insect stings, or other factors.
- Family History: Presence of similar symptoms in family members, which can indicate hereditary angioedema.
- Previous Episodes: Any previous occurrences of angioedema or related conditions like hives (urticaria).
- Medical Conditions: Existing medical conditions, especially autoimmune diseases, which can be associated with angioedema.
2. Physical Examination
A physical examination helps the healthcare provider assess the extent and characteristics of the swelling. This includes:
- Inspection: Visual examination of the affected areas.
- Palpation: Feeling the swollen areas to assess their firmness and tenderness.
3. Blood Tests
Blood tests can help identify underlying causes and rule out other conditions. Common tests include:
- Complete Blood Count (CBC): To check for signs of infection or inflammation.
- Complement Levels: Low levels of certain complement proteins (C4 and C1 inhibitor) can indicate hereditary angioedema.
- Allergy Tests: Specific IgE tests or skin prick tests can help identify allergic triggers.

4. Genetic Testing
For individuals suspected of having hereditary angioedema, genetic testing can confirm the diagnosis. This involves analyzing the C1 esterase inhibitor gene for mutations.
5. Imaging Studies
In some cases, imaging studies may be necessary to assess the extent of swelling or rule out other conditions:
- Ultrasound: To visualize internal structures and assess swelling in deeper tissues.
- CT or MRI Scans: Advanced imaging techniques may be used if the swelling affects internal organs or deeper tissues.
6. Medication Review
If medication-induced angioedema is suspected, a review of the patient’s medications is essential. The healthcare provider may recommend discontinuing the suspected medication to see if symptoms improve.
7. Skin Biopsy
In rare cases, a skin biopsy may be performed to examine tissue samples under a microscope. This can help rule out other skin conditions that may mimic angioedema.
8. Provocation Tests
For some individuals, controlled exposure to potential triggers under medical supervision may help identify the cause. This is done cautiously and only in a controlled environment.
Diagnosis of Specific Types of Angioedema
- Allergic: Typically diagnosed based on history, physical examination, and positive allergy tests.
- Hereditary (HAE): Diagnosed through complement level testing and genetic testing.
- Idiopathic: Diagnosed when no specific cause is identified after thorough evaluation.
- Medication-Induced: Diagnosed by identifying a temporal relationship between medication use and symptom onset.
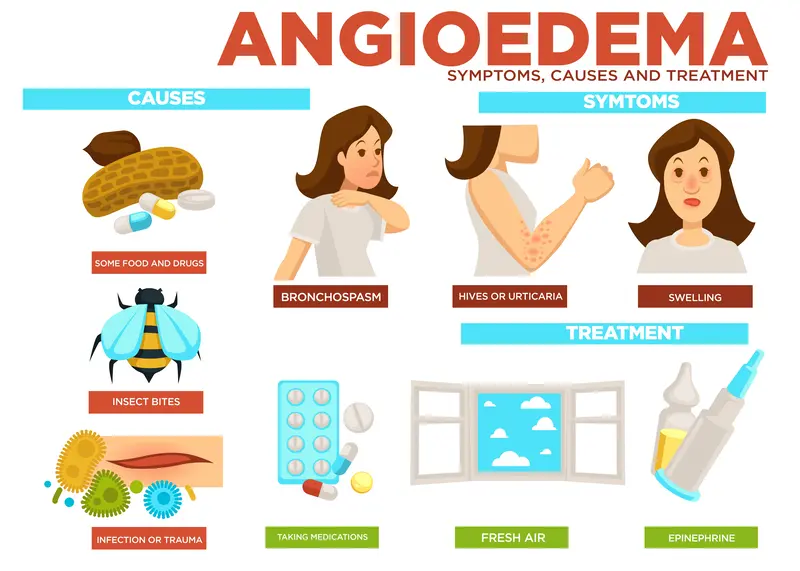
Treatment
The treatment aims to reduce symptoms during acute episodes, prevent recurrence, and manage underlying causes. The approach to treatment can vary depending on the type and severity.
1. Immediate Treatment for Acute Episodes
For acute episodes, the primary goal is to relieve symptoms and prevent complications, particularly those affecting the airway. Immediate treatments may include:
- Antihistamines: Antihistamines can help reduce swelling and alleviate symptoms, especially if the angioedema is caused by an allergic reaction.
- Examples: Diphenhydramine, cetirizine, loratadine
- Corticosteroids: Corticosteroids are often used to reduce inflammation and swelling in more severe cases.
- Examples: Prednisone, methylprednisolone
- Epinephrine (Adrenaline): In cases of severe angioedema, especially if there is difficulty breathing or swelling of the throat, an epinephrine injection is life-saving. This is typically administered through an auto-injector (e.g., EpiPen).
- Airway Management: In severe cases where the airway is compromised, emergency medical intervention may be required to secure the airway and ensure adequate breathing.
2. Long-Term Management and Prevention
For individuals with recurrent or chronic angioedema, long-term management focuses on preventing future episodes and addressing underlying causes:
- Avoidance of Triggers: Identifying and avoiding known triggers is crucial. This may involve dietary modifications, avoiding certain medications, or taking precautions against insect stings.
- Medication Review and Adjustment: If a medication is suspected as causative agents (e.g., ACE inhibitors), the healthcare provider may switch to an alternative medication.
- Prophylactic Medications: For those with frequent episodes, especially hereditary angioedema, prophylactic (preventive) medications may be prescribed:
- Androgens: Such as danazol or stanozolol, which help increase the production of C1 inhibitor protein.
- C1 Inhibitor Concentrates: Administered intravenously to prevent attacks in individuals with hereditary angioedema.
- Bradykinin Receptor Antagonists: Such as icatibant, which block the action of bradykinin, a protein involved in the inflammatory process.
- Plasma Kallikrein Inhibitors: Such as lanadelumab, which help prevent attacks by inhibiting plasma kallikrein.
- Immunosuppressants: In cases where angioedema is linked to autoimmune disorders, immunosuppressant medications may be used to reduce the immune system’s activity.
3. Lifestyle and Supportive Measures
- Emergency Action Plan: Having an action plan, including access to emergency medications like epinephrine, is crucial for individuals at risk of severe attacks.
- Medical Identification: Wearing a medical alert bracelet can help inform healthcare providers and emergency responders of the condition.
- Regular Monitoring: Regular follow-up appointments with a healthcare provider to monitor the condition and adjust treatment as needed.
- Education and Support: Educating patients and their families about the condition, its triggers, and management strategies. Support groups can also provide valuable resources and emotional support.
Living with Angioedema
It requires a proactive approach to manage the condition effectively:
- Emergency Plan: Have an action plan in place, including access to emergency medications like epinephrine.
- Medical Identification: Wearing a medical alert bracelet can help in emergencies.
- Regular Check-ups: Keep regular appointments with your healthcare provider to monitor the condition and adjust treatments as needed.
How To Reduce Angioedema Swelling at Home?
To reduce angioedema swelling at home:
- Cold Compress: Apply a cold compress to the affected area to reduce swelling and discomfort.
- Elevate Affected Area: Keep the swollen area elevated to help reduce swelling.
- Avoid Triggers: Identify and avoid known triggers, such as certain foods, medications, or environmental factors.
- Antihistamines: Take over-the-counter antihistamines like cetirizine or loratadine to reduce allergic reactions.
- Hydration: Drink plenty of water to stay hydrated and help flush out allergens.
- Rest: Ensure adequate rest to support your body’s healing process.
If symptoms persist or worsen, seek medical attention immediately!
Conclusion
Angioedema, while often alarming due to its sudden onset and potential severity, can be managed with appropriate treatment and preventive measures. Understanding the triggers, symptoms, and available treatments is crucial for individuals living with this condition. If you suspect you have angioedema, consult with a healthcare professional for an accurate diagnosis and tailored treatment plan. With the right approach, individuals can lead healthy, fulfilling lives.




