Malaria, a mosquito-borne infectious disease, remains a significant public health concern globally. While largely preventable and treatable, it continues to affect millions each year. This blog dives deep into the different types, how the disease develops, the warning signs and symptoms, diagnosis methods, treatment options, prevention strategies, and concludes with its global impact.
A Cast of Uninvited Guests: Types
Several Plasmodium parasites cause malaria in humans. The most common are:
- Plasmodium falciparum: The deadliest parasite, responsible for the most severe form.
- Plasmodium vivax: The most widespread parasite, causing recurrent episodes of disease.
- Plasmodium ovale: Less common, but can cause relapses similar to P. vivax.
- Plasmodium malariae: Another less common parasite, typically causing a milder form.
- Plasmodium knowlesi: Rare in humans, but increasingly reported in Southeast Asia.
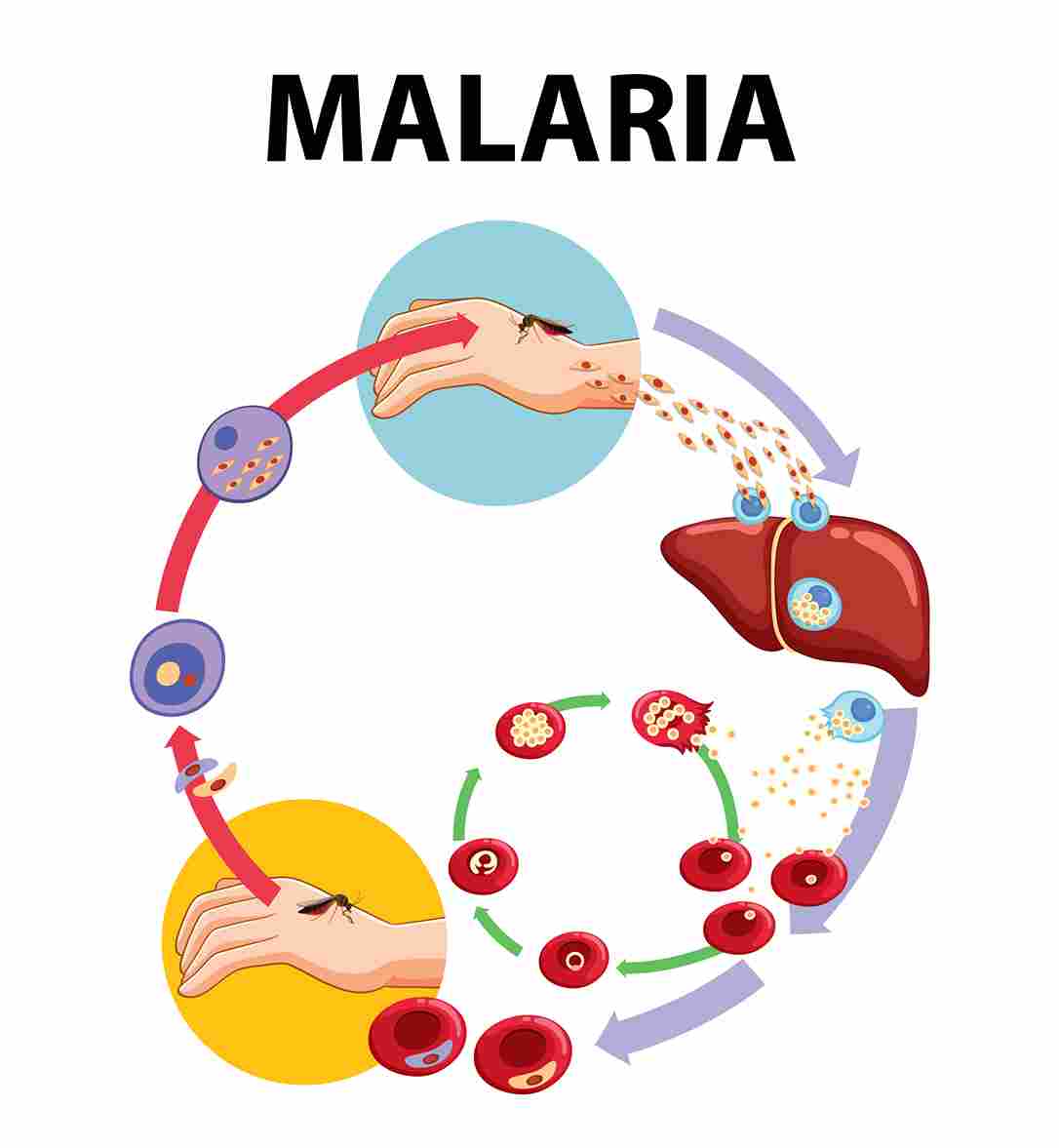
A Hostile Takeover: Pathogenesis
Life Cycle Of Malaria
It involves two hosts: humans and Anopheles mosquitoes. The process is complex and includes several stages:
1. Infection in Humans
A. Sporozoite Stage:
- Mosquito Bite: The life cycle begins when an infected female Anopheles mosquito bites a human, injecting Plasmodium sporozoites from its salivary glands into the bloodstream.
B. Liver Stage (Exoerythrocytic Stage):
- Liver Infection: The sporozoites travel to the liver, where they invade hepatocytes (liver cells).
- Schizogony: Inside the liver cells, the sporozoites mature into schizonts, which then rupture and release merozoites into the bloodstream. This stage lasts about 1-2 weeks, depending on the Plasmodium species.
- Hypnozoites: In the case of P. vivax and P. ovale, some sporozoites can become dormant in the liver as hypnozoites, causing relapses weeks, months, or even years later.
2. Blood Stage (Erythrocytic Stage)
A. Merozoite Stage:
- Red Blood Cell Invasion: The merozoites invade red blood cells (RBCs), where they undergo asexual reproduction (schizogony) again.
- Trophozoite Stage: Inside the RBCs, the merozoites develop into trophozoites, which mature into schizonts. The schizonts then rupture the RBCs, releasing new merozoites to infect more RBCs.
B. Gametocyte Stage:
- Sexual Forms: Some merozoites develop into sexual forms called gametocytes (male and female) instead of continuing the asexual cycle.
- Gametocyte Release: These gametocytes circulate in the bloodstream, awaiting uptake by another mosquito.
3. Infection in Mosquitoes
A. Gametogenesis:
- Mosquito Bite: When a mosquito bites an infected human, it ingests the gametocytes along with the blood.
- Gametocyte Activation: Inside the mosquito’s gut, the gametocytes develop into male and female gametes (microgametes and macrogametes).
B. Fertilization:
- Ookinete Formation: The male and female gametes fuse to form a zygote, which becomes a motile ookinete.
- Oocyst Formation: The ookinete penetrates the gut wall of the mosquito and forms an oocyst on the exterior side of the gut.
C. Sporogony:
- Sporozoite Production: Inside the oocyst, the parasite undergoes multiple divisions to produce numerous sporozoites.
- Oocyst Rupture: The oocyst bursts, releasing the sporozoites into the mosquito’s hemolymph (body cavity), from where they migrate to the salivary glands.
4. Cycle Repeats
- Transmission to Human: The mosquito, now carrying sporozoites in its salivary glands, bites another human, and the cycle begins anew.
Feeling Under the Weather? Signs and Symptoms
It can vary depending on the type of parasite and the severity of the infection. However, here are some common signs to watch for:
Flu-like symptoms:
- Fever and chills: This is the hallmark symptom , often occurring in cycles. Chills may precede a fever and can be quite severe.
- Headache: A frequent complaint.
General malaise:
- Muscle aches and fatigue: A general feeling of weakness and discomfort.
- Nausea and vomiting: May accompany other symptoms.
- Diarrhea: Can occur in some cases.
- Loss of appetite: Lack of interest in food.
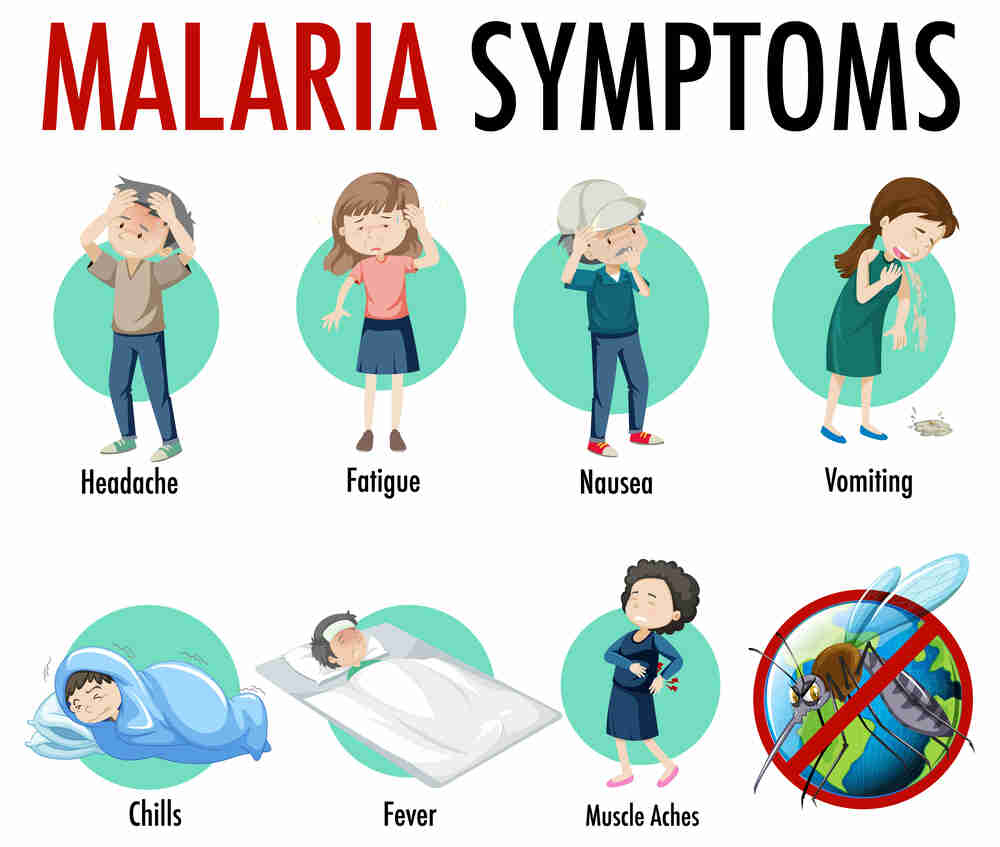
Other possible symptoms:
- Cough
- Jaundice (yellowing of the skin and whites of the eyes)
- Bleeding problems
- Seizures (in severe cases)
- Confusion (in severe cases)
- Coma (in severe cases)
Severe Malaria: P. falciparum infections can lead to severe disease, with complications like:
- Cerebral malaria: Affects the brain, causing confusion, seizures, and coma.
- Severe anemia: Destruction of red blood cells leads to a shortage of oxygen-carrying cells.
- Respiratory distress: Breathing difficulties can arise due to fluid buildup in the lungs.
- Kidney failure: It can damage the kidneys, affecting their function.
Remember: If you experience fever, chills, and other flu-like symptoms, especially after traveling to a endemic region, seek immediate medical attention. Early diagnosis and treatment are crucial for preventing severe complications.
Unveiling the Culprit: Diagnosis
It involves a two-pronged approach: identifying the presence of malarial parasites and determining the type of parasite causing the infection. Here’s a breakdown of the methods used:
Primary Diagnostic Tests:
-
Malaria peripheral blood smear: This is the gold standard in diagnosis. A thin and thick blood smear are prepared and examined under a microscope by a trained professional. The presence, type, and number of parasites within red blood cells can be identified.
-
Rapid Diagnostic Tests (RDTs): These are immunochromatographic tests that provide a quick and relatively accurate diagnosis. They detect specific antigens (proteins) of the malaria parasite in a blood sample. RDTs are particularly useful in areas with limited access to microscopy or when rapid diagnosis is crucial.
Additional Tests (may be used depending on circumstances):
-
Antibody Tests: These tests can detect antibodies (immune system proteins) produced in response to malarial infection. However, they cannot differentiate between an active infection and past exposure. Antibody tests might be used in conjunction with other tests or for epidemiological purposes.
-
PCR (Polymerase Chain Reaction) tests: These highly sensitive tests can detect very small amounts of parasite DNA in the blood. PCR tests are not routinely used for diagnosis due to their cost and complexity, but they can be helpful in certain situations, such as in cases of severe disease or when other tests are inconclusive.
Here are some additional points to consider:
- Importance of a qualified professional: Microscopic examination and interpretation of tests should be done by a trained healthcare professional to ensure accuracy.
- Limitations of RDTs: While convenient, RDTs may not be as sensitive as microscopy, particularly for detecting low parasite densities. False negatives are a possibility.
- Combined approach: In some cases, a combination of tests may be used for definitive diagnosis.
Battling the Parasite: Management
The management depends on the severity of the infection and the type of malaria parasite involved. Here’s a breakdown of the treatment approaches:
Uncomplicated Malaria:
-
Oral Antimalarial Medications: These are the mainstay of treatment for uncomplicated malaria. The specific medication used will depend on the type of parasite, local resistance patterns, and the patient’s medical history.
-
Examples of commonly used medications:
- Artemisinin-combination therapies (ACTs): These are used as first-line therapy globally. ACTs combine an artemisinin derivative (a fast-acting antimalarial drug) with another medication to prevent resistance development. Examples include artemether-lumefantrine (Coartem) and artesunate-amodiaquine.
- Other antimalarial medications like atovaquone-proguanil (Malarone) or chloroquine (depending on local resistance patterns) may be used in specific cases.
-
Supportive Care: Even with medication, patients with uncomplicated malaria may need supportive care to manage symptoms like fever, nausea, and dehydration. This may include:
- Fluids and electrolytes
- Pain relievers
- Antimalarial medications should be completed as prescribed by the healthcare professional, even if symptoms improve quickly. Incomplete treatment can lead to treatment failure and drug resistance.
Severe Malaria:
- Hospitalization is mandatory: Severe malaria, particularly caused by Plasmodium falciparum, is a medical emergency and requires immediate hospitalization.
- Intravenous Antimalarial Medications: These medications are administered directly into a vein for faster action. Artesunate is the first-line treatment.
- Supportive Care: Intensive supportive care is crucial in severe cases to manage complications like:
- Respiratory distress: Oxygen therapy may be needed.
- Kidney failure: Dialysis may be necessary.
- Cerebral malaria: Medications to reduce swelling in the brain may be used.
- Fluid and electrolyte imbalances: Intravenous fluids and electrolytes are essential.
- Blood sugar management: Monitoring and managing blood sugar levels is important.
Drug Resistance: An increasing concern is the emergence of resistance against some antimalarial medications. This highlights the importance of:
- Using antimalarial medications only as prescribed by a healthcare professional.
- Completing the full course of treatment even if symptoms improve.
Shielding Yourself: Effective Strategies for Prevention
Malaria, a mosquito-borne illness, remains a significant public health concern. While effective treatments exist, preventing infection in the first place is crucial. This blog empowering you to protect yourself and your loved ones.
Guarding Against Bites: Mosquito Control Measures
Mosquitoes are the primary culprits in transmission. Here’s how to minimize your exposure:
-
Insect Repellents: Apply insect repellents containing DEET (N,N-Diethyl-meta-toluamide) to exposed skin. Higher concentrations (20-35%) offer longer protection. Consider other EPA-registered repellents like picaridin, IR3535, or oil of lemon eucalyptus (OLE) if DEET is not preferred. Reapply repellent according to product instructions, especially after sweating or swimming.
-
Protective Clothing: Wear long-sleeved shirts, pants, and socks, particularly at dawn and dusk when mosquitoes are most active. Treat clothing with permethrin, a long-lasting insecticide (consult instructions for safe use).
-
Sleeping Arrangements: If sleeping outdoors in endemic areas, use mosquito nets treated with insecticide (permethrin or long-lasting insecticidal nets, LLNs). Ensure the net is tucked securely under your mattress. Consider staying in air-conditioned or well-screened accommodations whenever possible.
-
Indoor Residual Spraying (IRS): In some regions, public health programs implement IRS, spraying insecticides on the walls of homes to kill mosquitoes. This community-level approach can significantly reduce transmission.
Medications for Added Protection: Chemoprophylaxis
If you’re traveling to a malaria-endemic area, consider taking antimalarial medication as preventive therapy (chemoprophylaxis). Consult a healthcare professional or travel clinic well in advance of your trip to discuss:
- Destination: The specific parasite strains prevalent in your travel destination will influence medication choices.
- Medical History: Certain medications may interact with antimalarial, so disclose any existing medical conditions and medications you’re taking.
- Duration of Travel: The length of your trip will determine the appropriate chemoprophylaxis regimen.
Remember: Chemoprophylaxis is not a foolproof shield. It’s crucial to continue using mosquito bite prevention measures even while taking antimalarial medication.
Additional Preventive Strategies:
- Stay Informed: Before traveling, research the risk in your destination and the recommended preventive measures.
- Travel to Low-Risk Areas: If possible, prioritize travel to areas with low malaria transmission rates.
- Seek Prompt Medical Attention: If you experience fever, chills, or other malaria symptoms after returning from a endemic area, seek immediate medical attention. Early diagnosis and treatment are critical for preventing complications.
By employing these preventive measures, you can significantly reduce your risk of contacting malaria. Remember, prevention is the best defense against this potentially serious illness.
A Global Fight: The Impact of Malaria
It remains a significant global health concern:
- High Burden: Millions of cases occur annually, particularly in Africa, Southeast Asia, and South America.
- Disproportionate Impact: Children under five and pregnant women are most vulnerable to severe complications and death from malaria.
FAQs
What is malaria?
It is a serious and sometimes fatal disease caused by a parasite that commonly infects a certain type of mosquito which feeds on humans. People are typically very sick with high fevers, shaking chills, and flu-like illness.
What causes malaria?
It is caused by Plasmodium parasites, which are transmitted through the bites of infected female Anopheles mosquitoes. There are five species of Plasmodium parasites that can infect humans: P. falciparum, P. vivax, P. ovale, P. malariae, and P. knowlesi.
What are the symptoms of malaria?
Symptoms include fever, chills, headache, nausea and vomiting, muscle pain and fatigue, sweating, chest or abdominal pain, and cough. Severe malaria can cause seizures, coma, and death.
How is malaria diagnosed?
It is diagnosed through blood tests that can detect the presence of the parasite in the blood. These tests include microscopy, rapid diagnostic tests (RDTs), and molecular tests.
How can malaria be prevented?
Prevention includes avoiding mosquito bites through the use of insect repellent, wearing long sleeves and pants, using insecticide-treated bed nets, and taking antimalarial medications when traveling to areas where malaria is common.
Are there vaccines for malaria?
Yes, the RTS,S/AS01 (Mosquirix) is a vaccine that has been approved for use in some countries. It provides partial protection against malaria caused by Plasmodium falciparum, the most deadly species.
How is malaria treated?
It is treated with antimalarial medications. The choice of medication and length of treatment depend on the type of parasite, the severity of symptoms, and where the infection was acquired. Common treatments include chloroquine, artemisinin-based combination therapies (ACTs), and other antimalarial drugs.
where did malaria originate?
It originate in parts of Africa, South Asia, Central and South America, and the Pacific Islands. People living in or traveling to tropical and subtropical areas are at risk.
What are the complications of malaria?
Complications include severe anemia, cerebral malaria (which can cause seizures and coma), acute respiratory distress syndrome (ARDS), organ failure, and death.
What efforts are being made to combat malaria?
Efforts to combat include the distribution of insecticide-treated bed nets, indoor residual spraying, rapid diagnostic testing, effective antimalarial treatments, and ongoing research into vaccines and new treatment options.
Can pregnant women get malaria?
Yes, pregnant women are at higher risk of severe illness and complications, which can also affect the unborn child. Preventive measures and prompt treatment are crucial for pregnant women in endemic areas.
what are the isolation precautions for malaria
There are actually no specific isolation precautions. This is because it is not transmitted from person to person. Infact, they are transmitted through the bite of an infected mosquito. However, standard precautions should still be followed to prevent the spread of other germs and infections in a healthcare setting. Standard precautions include things like wearing gloves and gowns when caring for patients, washing hands frequently, and properly disposing of contaminated materials.



