Introduction
Corticosteroids, commonly referred to simply as steroids, are a class of medications that are widely used in medicine for their potent anti-inflammatory and immunosuppressive properties. They mimic the effects of hormones naturally produced by the adrenal glands. While these drugs can be life-saving and offer significant therapeutic benefits, they also come with a range of potential side effects. This blog delves into the basics of corticosteroids, their mechanisms of action, uses, and possible side effects.
Types
There are two main types of corticosteroids:
- Glucocorticoids: These target inflammation and immune system activity. Prednisone is a common example.
- Mineralocorticoids: These help regulate electrolytes and blood pressure. Fludrocortisone is an example.
How Corticosteroids Work
The primary mechanism of action for corticosteroids involves binding to specific intracellular glucocorticoid receptors. Here’s a step-by-step overview of how they work:
- Cell Entry: Corticosteroids pass through the cell membrane due to their lipophilic nature.
- Receptor Binding: Inside the cell, they bind to glucocorticoid receptors in the cytoplasm, forming a steroid-receptor complex.
- Nuclear Translocation: This complex then moves into the nucleus of the cell.
- Gene Regulation: In the nucleus, the complex binds to specific DNA sequences, influencing the transcription of certain genes. This results in increased production of anti-inflammatory proteins and decreased production of pro-inflammatory proteins.
By modulating gene expression, corticosteroids effectively reduce inflammation and suppress the immune system, providing relief from various inflammatory and autoimmune conditions.
How are Steroid Given?
Oral Administration
- Forms: Tablets, capsules, and liquid solutions.
- Common Uses: Chronic inflammatory conditions (like rheumatoid arthritis, asthma), autoimmune diseases, and certain allergic reactions.
- Examples: Prednisone, prednisolone, methylprednisolone.
Injectable Administration
- Intravenous (IV): Delivered directly into the bloodstream.
- Common Uses: Severe allergic reactions (anaphylaxis), acute asthma exacerbations, and other emergency conditions.
- Examples: Dexamethasone, hydrocortisone.
- Intramuscular (IM): Injected into a muscle.
-
- Common Uses: Long-acting treatment for chronic conditions, such as joint inflammation.
- Examples: Methylprednisolone acetate (Depo-Medrol), triamcinolone acetonide.
-
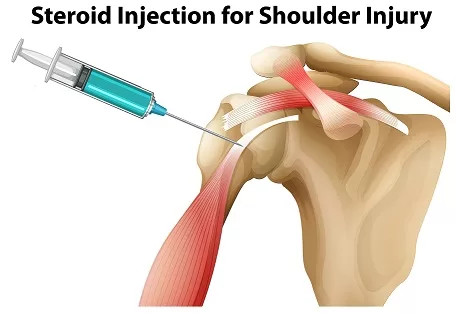
- Intra-articular (IA)corticosteroid injection: Injected directly into a joint.
- Common Uses: Localized joint inflammation, such as in osteoarthritis or rheumatoid arthritis.
- Examples: Triamcinolone, methylprednisolone.
- Epidural: Injected into the epidural space around the spinal cord.
- Common Uses: Severe back pain, sciatica.
- Advantages: Targeted pain relief.
- Examples: Methylprednisolone, triamcinolone.
Topical Administration
- Forms: Creams, ointments, gels, and lotions.
- Common Uses: Skin conditions like eczema, psoriasis, dermatitis.
- Examples: Hydrocortisone cream, betamethasone dipropionate.
Inhaled Administration
- Forms: Inhalers, nebulizers.
- Common Uses: Asthma, chronic obstructive pulmonary disease (COPD).
- Examples: Beclomethasone, fluticasone, budesonide.
Nasal Administration
- Forms: Nasal sprays.
- Common Uses: Allergic rhinitis, nasal polyps.
- Examples: Fluticasone, mometasone.
Ophthalmic Administration
- Forms: Eye drops, ointments.
- Common Uses: Eye inflammation, uveitis, post-surgical inflammation.
- Examples: Prednisolone acetate, dexamethasone.
Rectal Administration
- Forms: Suppositories, enemas, foams.
- Common Uses: Inflammatory bowel disease (ulcerative colitis).
- Examples: Hydrocortisone enema, budesonide rectal foam.
Uses of Corticosteroid
Corticosteroids are powerful medications used to treat a variety of conditions due to their anti-inflammatory and immunosuppressive properties. Here’s a comprehensive look at the primary uses of corticosteroids in clinical practice:
1. Anti-inflammatory Applications
Corticosteroids are widely used to reduce inflammation in various conditions:
- Asthma: Inhaled corticosteroids are the cornerstone of long-term asthma management.
- Chronic Obstructive Pulmonary Disease (COPD): Used to reduce inflammation and exacerbations.
- Allergic Rhinitis: Nasal corticosteroids help alleviate symptoms of nasal allergies.
2. Autoimmune and Inflammatory Disorders
Corticosteroids are effective in managing autoimmune and inflammatory diseases:
- Rheumatoid Arthritis: To reduce joint inflammation and pain.
- Systemic Lupus Erythematosus: To manage flare-ups and systemic involvement.
- Inflammatory Bowel Disease (IBD): Including Crohn’s disease and ulcerative colitis, to reduce intestinal inflammation.
- Multiple Sclerosis: Used during acute relapses to decrease inflammation and neurological damage.
3. Allergic Reactions
For severe allergic reactions, corticosteroids can be life-saving:
- Anaphylaxis: Used in combination with epinephrine and other medications.
- Severe Dermatitis: Including eczema and contact dermatitis, to reduce inflammation and itching.
- Drug Allergies: To manage severe allergic reactions to medications.
4. Dermatological Conditions
Topical corticosteroids are commonly used for various skin conditions:
- Psoriasis: To reduce plaques and inflammation.
- Eczema: To relieve itching and inflammation.
- Dermatitis: Including atopic and contact dermatitis, for symptom control.
5. Endocrine Disorders
Corticosteroids are used in hormone replacement therapy for adrenal insufficiency:
- Addison’s Disease: For replacing deficient cortisol.
- Congenital Adrenal Hyperplasia: To replace deficient hormones and manage symptoms.
6. Oncological Applications
In cancer treatment, corticosteroids serve several roles:
- Chemotherapy-Induced Nausea and Vomiting: Used in combination with other antiemetics.
- Brain Tumors: To reduce edema and intracranial pressure.
- Lymphoma and Leukemia: Part of chemotherapy regimens for certain types of cancer.
7. Organ Transplantation
Corticosteroids are critical in preventing organ rejection:
- Immunosuppression: To prevent the body from rejecting transplanted organs, often used in combination with other immunosuppressive drugs.
8. Respiratory Disorders
Besides asthma and COPD, corticosteroids are used in other respiratory conditions:
- Sarcoidosis: To reduce inflammation in affected organs.
- Pneumonia: In severe cases, such as Pneumocystis pneumonia in immunocompromised patients.
9. Neurological Conditions
Corticosteroids help manage inflammation in the nervous system:
- Acute Spinal Cord Injury: To reduce swelling and improve outcomes.
- Meningitis: Certain types of meningitis benefit from corticosteroid therapy to reduce inflammation and complications.
10. Other Medical Conditions
Corticosteroids have diverse applications in various other conditions:
- Eye Disorders: Such as uveitis and optic neuritis, to reduce inflammation.
- Hematologic Disorders: Including idiopathic thrombocytopenic purpura (ITP) to increase platelet count.
- Nephrotic Syndrome: To reduce proteinuria and kidney inflammation.
Corticosteroid Potency Chart
Corticosteroids vary in their potency, which determines the dosage needed to achieve the desired therapeutic effect. Potency is typically classified into three main categories: low, medium, and high. This chart provides a general overview of the potency levels of various corticosteroids.
Low Potency Corticosteroids
These are typically used for mild conditions and are often the first line of treatment due to their lower risk of side effects.
| Drug Name | Brand Name | Formulations | Relative Potency |
|---|---|---|---|
| Hydrocortisone | Cortef | Oral, topical, injectable | 1 |
| Prednisolone | Orapred, Prelone | Oral | 4 |
| Methylprednisolone | Medrol | Oral, injectable | 5 |
| Dexamethasone | Decadron | Oral, topical, injectable | 25 |
Medium Potency Corticosteroids
These are used for moderate conditions or when low potency corticosteroids are not effective.
| Drug Name | Brand Name | Formulations | Relative Potency |
|---|---|---|---|
| Triamcinolone | Kenalog | Oral, topical, injectable | 5 |
| Prednisone | Deltasone | Oral | 4 |
| Fludrocortisone | Florinef | Oral | 10 |
High Potency Corticosteroids
High potency corticosteroids are reserved for severe conditions or when medium potency drugs fail to achieve the desired effect.
| Drug Name | Brand Name | Formulations | Relative Potency |
|---|---|---|---|
| Betamethasone | Celestone | Oral, topical, injectable | 25 |
| Clobetasol | Clobex | Topical | 600 |
| Diflorasone diacetate | Psorcon | Topical | 50 |
| Fluocinonide | Lidex | Topical | 50 |
Notes on Potency and Usage
- Relative Potency: The potency of corticosteroids is often compared to hydrocortisone, which has a relative potency of 1. Higher numbers indicate greater potency.
- Formulations: Corticosteroids are available in various formulations including oral tablets, topical creams and ointments, and injectable solutions. The choice of formulation depends on the condition being treated.
- Topical Potency: Topical corticosteroids are specifically formulated for skin conditions. Their potency can significantly affect their safety and effectiveness.
- Systemic Effects: Oral and injectable forms can have systemic effects, impacting the entire body, whereas topical forms generally have localized effects but can still be absorbed systemically, especially with high potency formulations or extensive use.
Corticosteroid Tapering Guidelines
Tapering off corticosteroids is a crucial process to prevent withdrawal symptoms and allow the adrenal glands to resume their normal function after prolonged corticosteroid therapy. Abruptly stopping corticosteroids can lead to adrenal insufficiency, which can be life-threatening. Here are general guidelines for corticosteroid tapering, but always consult with a healthcare provider for personalized advice.
Why Taper Corticosteroids?
- Prevent Withdrawal Symptoms: Sudden discontinuation can cause symptoms like fatigue, body aches, and joint pain.
- Adrenal Gland Recovery: Long-term corticosteroid use can suppress the hypothalamic-pituitary-adrenal (HPA) axis, leading to reduced endogenous cortisol production.
- Minimize Flare-Ups: Gradually reducing the dose helps prevent the return of the underlying condition being treated.
General Tapering Guidelines
- Duration of Tapering: The tapering schedule depends on the duration and dosage of corticosteroid therapy. Longer and higher-dose treatments require more gradual tapering.
- Initial Reduction: Start by reducing the dose by 10-20% every 1-2 weeks.
- Dose Adjustments: Monitor patient symptoms closely. If withdrawal symptoms or a flare of the underlying condition occur, slow the taper or increase the dose slightly before resuming tapering.
- Final Stages: When approaching physiological doses (equivalent to the body’s natural cortisol production, about 5-7.5 mg of prednisone per day), taper more slowly, often by 1 mg every 1-2 weeks.
Example Tapering Schedule
Here’s a generic example of a tapering schedule for a patient who has been on 40 mg of prednisone daily for several weeks:
- Week 1-2: Reduce to 30 mg per day
- Week 3-4: Reduce to 20 mg per day
- Week 5-6: Reduce to 15 mg per day
- Week 7-8: Reduce to 10 mg per day
- Week 9-10: Reduce to 7.5 mg per day
- Week 11-12: Reduce to 5 mg per day
- Week 13-14: Reduce to 2.5 mg per day
- Week 15-16: Stop or reduce to 1 mg every other day before stopping
Special Considerations
- Long-term Therapy: For those on corticosteroids for more than a year, tapering might need to extend over months.
- Short-term High Dose: If corticosteroids were used for less than three weeks, a faster taper might be acceptable.
- Underlying Conditions: Consider the underlying condition being treated. For autoimmune diseases, a slower taper may help prevent flare-ups.
- Individual Response: Adjust the tapering schedule based on patient response, both physically and psychologically.
- Alternate-Day Dosing: In some cases, alternate-day dosing can help reduce side effects and support adrenal recovery.
Monitoring and Support
- Regular Follow-Ups: Schedule regular follow-ups to monitor symptoms and adrenal function.
- Patient Education: Inform patients about potential withdrawal symptoms and the importance of adherence to the tapering schedule.
- Lab Tests: Periodic blood tests to assess adrenal function, including ACTH stimulation tests, may be necessary.
- Supplemental Therapy: In some cases, supplemental therapies like hydrocortisone may be used during the tapering process.
Side Effects of Corticosteroids
While corticosteroids are effective in treating a wide range of conditions, they can cause a variety of side effects, especially when used long-term or at high doses. Understanding these potential side effects is crucial for managing risks and ensuring safe use. Here’s a comprehensive overview of the side effects associated with corticosteroids:
Common Side Effects
-
Metabolic Effects
- Weight Gain: Increased appetite and fluid retention can lead to weight gain.
- Redistribution of Body Fat: Fat deposits may develop in the abdomen, face (moon face), and upper back (buffalo hump).
-
Musculoskeletal Effects
- Osteoporosis: Long-term use can lead to bone thinning, increasing the risk of fractures.
- Muscle Weakness: Steroid myopathy, or muscle weakness, can occur, especially in the legs.
-
Gastrointestinal Effects
- Peptic Ulcers: Increased risk of developing stomach ulcers.
- Pancreatitis: Inflammation of the pancreas, which can be severe.
-
Cardiovascular Effects
- Hypertension: Increased blood pressure due to fluid retention.
- Increased Risk of Cardiovascular Disease: Long-term use may increase the risk of heart attacks and strokes.
-
Endocrine Effects
- Hyperglycemia: Elevated blood sugar levels, which can lead to or worsen diabetes.
- Suppression of Adrenal Gland Hormone Production: Long-term use can suppress the body’s ability to produce cortisol naturally.
-
Dermatological Effects
- Skin Thinning and Easy Bruising: Skin becomes more fragile and susceptible to injury.
- Acne: Increased risk of acne and other skin infections.
-
Immunosuppression
- Increased Susceptibility to Infections: Higher risk of infections due to suppressed immune response.
- Delayed Wound Healing: Slower healing of cuts, bruises, and other injuries.
-
Ophthalmic Effects
- Cataracts: Long-term use can increase the risk of developing cataracts.
- Glaucoma: Elevated intraocular pressure can lead to glaucoma.
-
Psychiatric Effects
- Mood Swings: Changes in mood, including irritability and euphoria.
- Depression and Anxiety: Increased risk of mental health issues.
- Steroid-Induced Psychosis: Severe cases may involve hallucinations and delusions.
Long-term Side Effects
- Cushingoid Appearance
- Prolonged use can lead to Cushing’s syndrome, characterized by a round face, abdominal obesity, and purple stretch marks.
- Growth Suppression in Children
- Long-term use can inhibit growth in children, requiring careful monitoring.
- Bone Density Loss
- Chronic use can lead to significant bone density loss, necessitating preventive measures like calcium and vitamin D supplements.
Management and Prevention of Side Effects
- Dosage and Duration: Use the lowest effective dose for the shortest possible duration to minimize side effects.
- Monitoring: Regular monitoring of blood pressure, blood sugar, bone density, and eye health.
- Supplementation: Calcium and vitamin D supplements to prevent osteoporosis, and medications like bisphosphonates if necessary.
- Lifestyle Modifications: Healthy diet, regular exercise, and avoiding smoking and excessive alcohol.
- Alternate-Day Therapy: For some conditions, alternate-day dosing can reduce side effects.
- Tapering: Gradually reducing the dose rather than abrupt cessation to avoid withdrawal symptoms and allow adrenal recovery.
- Regular Check-Ups: Frequent visits to the healthcare provider for early detection and management of side effects.
Conclusion
Corticosteroids are powerful medications that play a crucial role in managing a variety of medical conditions. Their ability to reduce inflammation and suppress the immune system makes them indispensable in many therapeutic protocols. However, due to their broad range of potential side effects, their use must be carefully managed by healthcare professionals. Understanding the balance between the benefits and risks of corticosteroids is essential for optimizing treatment outcomes and ensuring patient safety.
Always consult with a healthcare provider before starting or stopping corticosteroid therapy to ensure it is used safely and effectively.