Implantable Cardioverter-Defibrillators (ICDs) are sophisticated medical devices designed to monitor and treat life-threatening heart arrhythmias. These remarkable devices serve as a critical lifeline for individuals at risk of sudden cardiac death.
Purpose And Functionality of ICD:
ICDs are primarily used to manage and treat ventricular arrhythmias, particularly ventricular tachycardia (VT) and ventricular fibrillation (VF). These arrhythmias can lead to cardiac arrest and, if not addressed promptly, may result in sudden death. It are equipped with several essential features:
-
Arrhythmia Detection :
ICDs continuously monitor the heart’s electrical activity. When they detect a life-threatening arrhythmia, they respond rapidly to correct it.
-
Defibrillation:
If VF occurs, the Implantable cardioverter defibrillator delivers a high-energy electric shock to the heart, restoring a normal rhythm. This is known as defibrillation and is crucial in preventing sudden cardiac death.
-
Anti-Tachycardia Pacing:
For VT, ICDs can deliver rapid pacing pulses to terminate the arrhythmia without the need for a shock. This is called anti-tachycardia pacing (ATP).
-
Bradycardia Support:
Many ICDs also incorporate pacemaker functions to address bradycardia (slow heart rhythms) if they occur.
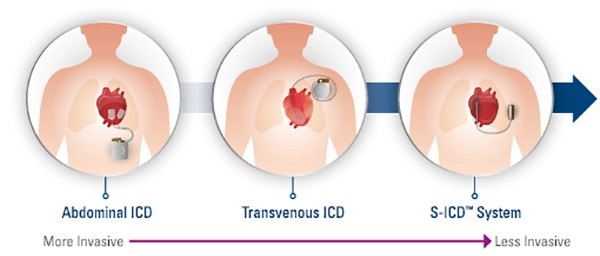
Types of ICDs :
Indications of ICDs :
Implantable Cardioverter-Defibrillators (ICDs) are recommended for individuals who are at risk of life-threatening ventricular arrhythmias, specifically ventricular tachycardia (VT) and ventricular fibrillation (VF). The decision to implant an ICD is typically based on established clinical guidelines and individual patient characteristics. Here are some of the primary indications for ICD implantation:
- Secondary Prevention:
- Survivors of Sudden Cardiac Arrest (SCA): Individuals who have survived a sudden cardiac arrest episode due to VT or VF should receive an ICD. This is known as secondary prevention, and it aims to prevent future episodes of SCA.
- Primary Prevention:
- Reduced Left Ventricular Ejection Fraction (LVEF): Patients with specific heart conditions, such as ischemic or non-ischemic cardiomyopathy, who have a reduced LVEF below a certain threshold (typically ≤35% or ≤30%) and are at risk of arrhythmic events may be candidates for primary prevention ICDs. The goal is to prevent sudden cardiac death before it occurs.
- Specific Arrhythmia Conditions:
- High-Risk Brugada Syndrome: Individuals with Brugada syndrome, a genetic condition associated with ventricular arrhythmias, may benefit from an ICD if they have certain risk factors.
- Arrhythmogenic Right Ventricular Dysplasia (ARVD): In ARVD, ICDs can be considered for patients at high risk of ventricular arrhythmias.
- Certain Inherited Conditions:
- Long QT Syndrome (LQTS) and Hypertrophic Cardiomyopathy (HCM): Some individuals with these inherited cardiac conditions may require an ICD if they have specific risk factors or a history of arrhythmias.
- Bridge to Heart Transplantation: Patients with advanced heart failure who are awaiting heart transplantation may receive an ICD as a bridge to transplantation to manage arrhythmias and support heart function until a donor heart becomes available.
- Other Clinical Criteria:
- Myocardial Infarction (Heart Attack): In some cases, ICD implantation might be considered for individuals who have had a heart attack and meet certain criteria.
- Non-Ischemic Cardiomyopathy: Patients with non-ischemic cardiomyopathy and specific risk factors may be candidates for ICDs.
- Prior History of VT or VF: Individuals who have experienced documented VT or VF in the past and are considered at high risk of recurrence may receive an ICD.
It’s important to note that ICD implantation decisions are individualized and should be made by a cardiac electrophysiologist or cardiologist with expertise in arrhythmia management. These specialists consider a patient’s medical history, clinical condition, risk factors, and other relevant factors when determining whether an ICD is appropriate. The goal is to balance the potential benefits of ICD therapy in preventing sudden cardiac death with the risks associated with the device and the procedure itself
Benefits of ICDs :
Implantable Cardioverter-Defibrillators offer numerous benefits to patients with a high risk of life-threatening arrhythmias:
- Sudden Cardiac Death Prevention: The primary benefit of ICDs is their ability to prevent sudden cardiac death. When they detect VT or VF, which can lead to cardiac arrest, ICDs deliver a life-saving electric shock (defibrillation) to restore a normal heart rhythm. This intervention can be performed within seconds and is often the only effective treatment for such arrhythmias.
- Increased Survival Rates: Studies have shown that ICDs significantly increase the chances of survival for individuals at risk of sudden cardiac death. These devices have saved countless lives by promptly and effectively treating life-threatening arrhythmias.
- Improved Quality of Life: For people with recurrent or symptomatic ventricular arrhythmias, ICDs can offer peace of mind and an improved quality of life. Knowing that the device is continuously monitoring their heart and ready to intervene if necessary can reduce anxiety and allow them to resume their daily activities with confidence.
- Customizable Therapy: ICDs can be programmed to deliver various types of therapy, such as high-energy shocks, anti-tachycardia pacing (ATP), or bradycardia support, depending on the patient’s specific needs. This customization ensures that therapy is tailored to the individual’s condition.
- Remote Monitoring: Many modern ICDs are equipped with remote monitoring capabilities. This means that healthcare providers can remotely access the device’s data, including heart rhythm information, device integrity, and battery status. Remote monitoring allows for timely detection of issues and adjustments to device settings, reducing the need for frequent in-person clinic visits.
- Long-Term Protection: ICDs are designed to provide long-term protection, reducing the risk of recurrent life-threatening arrhythmias. This can lead to fewer hospitalizations related to arrhythmias, ultimately improving the patient’s overall well-being.
- Bridge to Heart Transplantation: In some cases, ICDs can serve as a bridge to heart transplantation for individuals with end-stage heart failure. They help maintain heart function while the patient awaits a suitable donor heart.
- Evidence-Based Guidelines: The use of ICDs is guided by evidence-based guidelines and clinical criteria. This ensures that they are implanted in individuals who are most likely to benefit from them, optimizing their effectiveness.
Implantation Procedure :
The implantation is typically performed by a skilled cardiologist or cardiac electrophysiologist in a sterile environment, often in a cardiac catheterization laboratory or operating room. The procedure involves several key steps:
-
- Arrhythmia Detection: ICDs continuously monitor the heart’s electrical activity. When they detect a life-threatening arrhythmia, they respond rapidly to correct it.
- Defibrillation: If VF occurs, the ICD delivers a high-energy electric shock to the heart, restoring a normal rhythm. This is known as defibrillation and is crucial in preventing sudden cardiac death.
- Anti-Tachycardia Pacing: For VT, ICDs can deliver rapid pacing pulses to terminate the arrhythmia without the need for a shock. This is called anti-tachycardia pacing (ATP).
- Bradycardia Support: Many ICDs also incorporate pacemaker functions to address bradycardia (slow heart rhythms) if they occur. Anesthesia : Local anesthesia is administered to numb the implantation area, which is usually near the left or right collar bone
- Lead Placement: Thin, insulated wires (leads) are inserted through a vein and advanced into the heart. These leads sense the heart’s electrical activity and deliver electrical impulses or shocks when necessary. One or more leads may be used, depending on the specific device and the patient’s needs.
- ICD Placement: The ICD device, which contains the battery, control unit, and necessary electronics, is implanted under the skin, typically below the collarbone. The leads are connected to the device.
- Testing: The system is tested to ensure proper lead positioning and device functionality. Specialized equipment is used to induce and terminate arrhythmias, ensuring the ICD responds appropriately.
- Closure: The incision is closed, and the wound is sutured.
Complication of Implant :
ICD implantation can be a life-saving procedure, there can be complications associated with the placement and use of these devices. Here are some potential complications of ICD implantation:
- Infection : Infections can occur at the surgical site or along the leads (wires) that connect the device to the heart. Signs of infection may include fever, redness, swelling, or drainage at the implant site.
- Bleeding or hematoma: During the implantation procedure, there is a risk of bleeding, which can lead to the formation of a hematoma (a collection of blood outside a blood vessel). This can cause pain and swelling at the implant site.
- Lead-related issues: The leads that connect the ICD to the heart may become dislodged, fractured, or damaged over time. This can result in inappropriate shocks, loss of therapy, or the need for lead revision or replacement.
- Pneumothorax: The insertion of leads into the heart can sometimes puncture the lung, leading to a pneumothorax (collapsed lung). Symptoms include chest pain and difficulty breathing.
- Device-related complications: ICDs can malfunction or experience technical issues, such as battery depletion, electrode problems, or programming errors.
- Allergic reactions or sensitivity: Some individuals may experience allergic reactions or skin sensitivity to materials in the device or the surgical sutures used to close the incision.
- Scar tissue formation: Over time, scar tissue can form around the leads or the device, potentially interfering with device function or making future device revisions more challenging.
- Device pocket complications: The device is typically placed in a “pocket” created under the skin, and issues such as pocket infection, erosion, or hematoma can occur.
- Pain or discomfort: Some individuals may experience pain, discomfort, or muscle twitching near the device implant site.
- Inappropriate shocks: Occasionally, the ICD may deliver shocks when they are not needed, which can be uncomfortable and frightening.
- Psychological impact: Living with an ICD can cause anxiety, stress, or psychological distress, especially when patients are concerned about the possibility of receiving a shock.
- Complications from anesthesia: Like any surgical procedure, ICD implantation carries risks associated with anesthesia, including allergic reactions, respiratory problems, or adverse reactions to medications.
It’s important to note that the benefits of ICD implantation often outweigh the risks for individuals at high risk of life-threatening arrhythmias. Patients should discuss the potential risks and benefits of the procedure with their healthcare team and carefully follow up with their healthcare provider for routine device checks and monitoring to detect and address any complications early.
Conclusion :
Implantable Cardioverter-Defibrillators are vital medical devices that have revolutionized the management of life-threatening heart arrhythmias. These devices offer a combination of early detection, rapid intervention, and long-term protection, ultimately enhancing the quality of life for patients at risk of sudden cardiac death.

Frequently Asked Questions (FAQs) ;
What is an ICD and why is it used?
An ICD is a small electronic device implanted under the skin, typically near the collarbone, to continuously monitor heart rhythms and deliver electrical shocks to restore normal rhythm if dangerous irregularities are detected.
Why do people need ICD?
ICDs are typically recommended for people who are at risk of sudden cardiac arrest due to life-threatening heart rhythm disorders such as ventricular tachycardia or ventricular fibrillation. This includes individuals with a history of heart attack, certain inherited heart conditions, or those at high risk of arrhythmias.
What is the working mechanism of ICD?
The device continuously monitors the heart's electrical activity. If it detects an abnormal heart rhythm, it can deliver either pacing pulses or electrical shocks to restore normal rhythm. Some ICDs also have the capability to act as pacemakers, providing regular pacing if the heart rate becomes too slow.
Is getting an ICD implantation procedure risky?
Like any surgical procedure, there are risks associated with ICD implantation, such as infection, bleeding, or device-related complications. However, the procedure is generally considered safe, and the benefits of having an ICD often outweigh the risks for individuals at high risk of sudden cardiac death.
Can you live a normal life with a pacemaker?
In most cases, yes. Many people with ICDs can lead normal, active lives with some precautions. It's important to discuss any specific concerns or lifestyle adjustments with your healthcare provider.
What is a limitation of a patient with an ICD?
Activities that involve strong electromagnetic fields, such as certain medical procedures, industrial equipment, or high-voltage machinery, may need to be approached with caution. Additionally, some sports and activities with a risk of physical impact may require modification or avoidance to prevent damage to the device or leads.
Do ICDs require regular maintenance?
Yes, ICDs require regular monitoring and periodic follow-up appointments with your healthcare provider to ensure the device is functioning properly and to adjust settings as needed. This may involve remote monitoring via wireless technology or in-person visits.
What should I do if I feel a shock from my ICD?
If you receive a shock from your ICD, it's important to seek medical attention immediately, even if you feel fine afterward. Your healthcare provider will evaluate the situation to determine the cause of the shock and whether any adjustments to your device or treatment plan are necessary.
Is it OK to travel with pacemaker?
Yes, most people with ICDs can travel safely. However, it's recommended to inform airport security personnel about your device before undergoing security screening, as the device may trigger metal detectors or security scanners. Additionally, it's a good idea to carry a copy of your device identification card and contact information for your healthcare provider when traveling.
What are the potential complications associated with having an ICD?
Complications from having an ICD are relatively rare but can include infection, bleeding, lead dislodgement, device malfunction, or inappropriate shocks. It's important to promptly report any symptoms or concerns to your healthcare provider.



