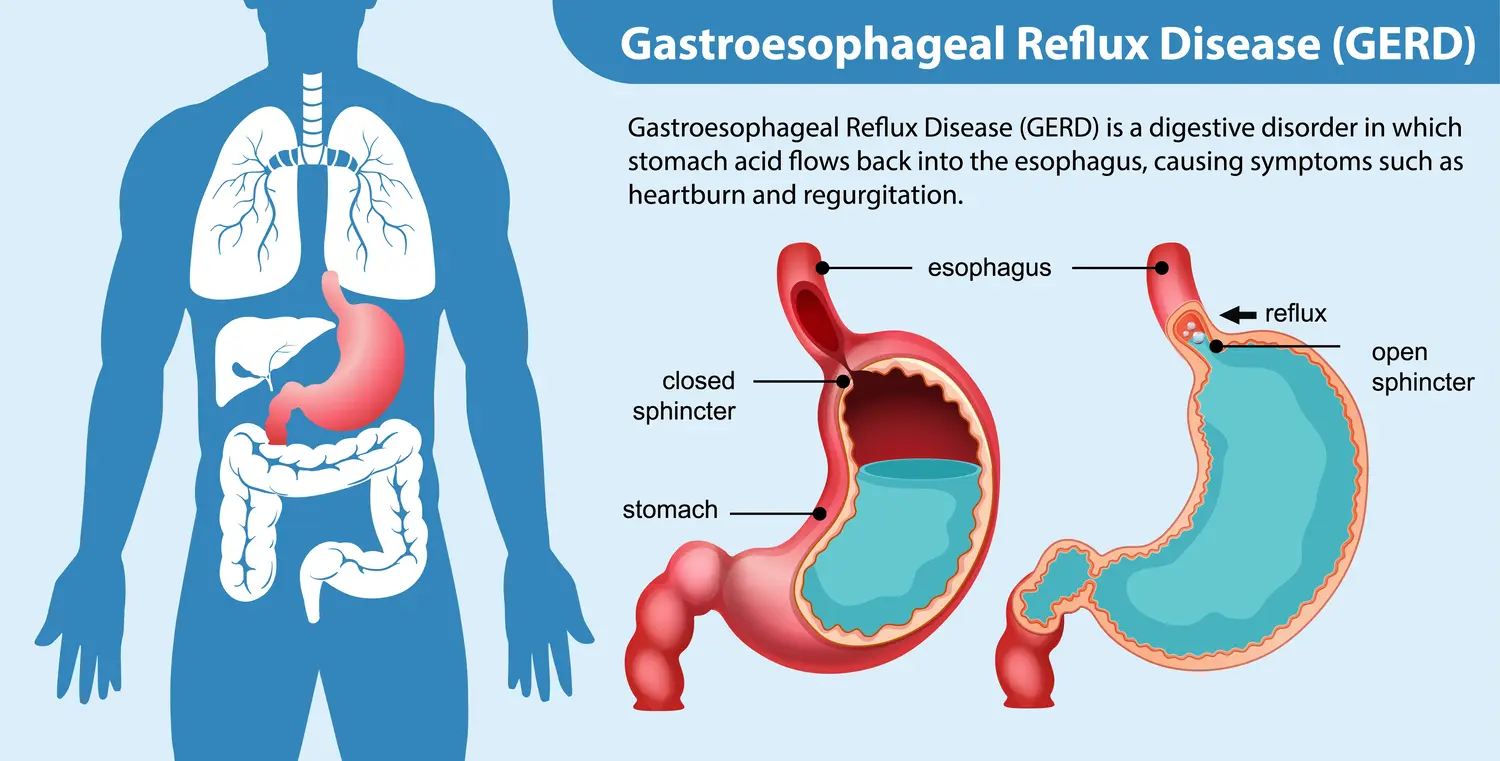
Esophageal reflux, commonly known as gastroesophageal reflux disease (GERD), is a condition where stomach acid frequently flows back into the esophagus, the tube connecting your mouth and stomach. This backwash, or acid reflux, can irritate the lining of your esophagus and cause various symptoms.
Pathophysiology
The pathophysiology of gastroesophageal reflux disease (GERD) involves multiple mechanisms that result in the reflux of stomach contents, including acid and bile, into the esophagus. This reflux leads to the characteristic symptoms of GERD and can cause damage to the esophageal lining.
Key Components of GERD Pathophysiology:
- Lower Esophageal Sphincter (LES) Dysfunction:
- Primary Factor: The LES is a circular muscle at the junction between the esophagus and stomach. Its primary function is to act as a barrier, preventing stomach contents from flowing back into the esophagus.
- Inappropriate Relaxation: In GERD, the LES may relax inappropriately, either spontaneously or in response to certain triggers (e.g., food, alcohol, caffeine), leading to reflux.
- Weak LES Pressure: A chronically weak LES can fail to maintain adequate closure pressure, making reflux more likely, especially when lying down or after meals.
- Transient LES Relaxations (TLESRs):
- Temporary LES Relaxation: TLESRs are brief relaxations of the LES that are not related to swallowing. These episodes are a normal physiological response to gastric distention but are exaggerated in people with GERD, leading to increased acid reflux episodes.
- Hiatal Hernia:
- Anatomical Defect: A hiatal hernia occurs when part of the stomach protrudes through the diaphragm into the chest cavity. This can disrupt the normal functioning of the LES, making it easier for stomach acid to reflux into the esophagus.
- Impaired Diaphragm Support: The diaphragm normally aids the LES in preventing reflux. A hiatal hernia reduces this support, contributing to GERD.
- Impaired Esophageal Clearance:
- Reduced Peristalsis: Normally, the esophagus clears refluxed acid through coordinated muscle contractions known as peristalsis. In GERD, peristalsis may be weakened or disorganized, allowing acid to remain in the esophagus longer.
- Reduced Saliva Production: Saliva helps neutralize and clear acid from the esophagus. Reduced saliva production (e.g., due to smoking or certain medications) can impair this protective mechanism.
- Delayed Gastric Emptying (Gastroparesis):
- Slow Stomach Emptying: When the stomach takes longer to empty its contents, the increased volume and pressure can promote reflux. Conditions like gastroparesis (often seen in diabetes) can contribute to this delayed emptying.
- Increased Intra-Abdominal Pressure:
- Factors That Increase Pressure: Obesity, pregnancy, tight clothing, or overeating can increase intra-abdominal pressure, pushing stomach contents upwards into the esophagus.
- Refluxed Material:
- Acid and Bile: The refluxed material typically contains hydrochloric acid, pepsin (a digestive enzyme), and sometimes bile. These substances can damage the esophageal lining, leading to inflammation, ulceration, and the symptoms of GERD.
- Esophageal Mucosal Defense:
- Mucosal Resistance: The esophageal lining has certain protective mechanisms (e.g., mucus production, tight junctions between cells) to resist acid damage. In GERD, these defenses can be overwhelmed, leading to esophagitis (inflammation of the esophagus).
- Sensitivity to Acid: Chronic acid exposure can increase the sensitivity of the esophageal lining, leading to more pronounced symptoms even with small amounts of acid.
- Neural and Hormonal Factors:
- Vagus Nerve: The vagus nerve plays a role in regulating LES tone and gastric acid secretion. Abnormalities in vagal function can contribute to GERD.
- Hormonal Influences: Hormones like progesterone (elevated during pregnancy) can relax the LES, increasing the risk of reflux.
Causes
GERD (Gastroesophageal Reflux Disease) is caused by a combination of lifestyle factors, physiological conditions, and certain foods or habits that can weaken the lower esophageal sphincter (LES), the muscle that controls the passage between the esophagus and the stomach. When the LES is weak or relaxes inappropriately, stomach acid can flow back into the esophagus, leading to the symptoms of GERD.
Common Causes of GERD:
- Weak or Dysfunctional Lower Esophageal Sphincter (LES):
- The LES is a ring of muscle that acts as a valve between the esophagus and the stomach. If it becomes weak or relaxes when it shouldn’t, stomach acid can escape into the esophagus.
- Hiatal Hernia:
- A condition where part of the stomach pushes up through the diaphragm into the chest cavity. This can weaken the LES and increase the likelihood of acid reflux.
- Obesity:
- Excess body weight, especially around the abdomen, can increase pressure on the stomach, forcing stomach contents, including acid, back up into the esophagus.
- Pregnancy:
- Hormonal changes during pregnancy can relax the LES, and the growing fetus can put pressure on the stomach, increasing the risk of acid reflux.
- Smoking:
- Smoking weakens the LES, reduces saliva production (which helps neutralize acid), and increases stomach acid production.
- Certain Foods and Drinks:
- Fatty Foods: High-fat foods can relax the LES.
- Spicy Foods: Can irritate the esophagus.
- Chocolate: Contains caffeine and theobromine, which can relax the LES.
- Caffeine: Found in coffee, tea, and some sodas, can relax the LES.
- Alcohol: Relaxes the LES and increases stomach acid production.
- Citrus Fruits and Juices: Highly acidic and can irritate the esophagus.
- Tomato-Based Products: Acidic and can cause reflux.
- Eating Large Meals or Lying Down After Eating:
- A full stomach can put pressure on the LES, especially if you lie down shortly after eating, making it easier for acid to back up into the esophagus.
- Delayed Stomach Emptying (Gastroparesis):
- A condition where the stomach takes longer to empty its contents, increasing the risk of acid reflux.
- Medications:
- Certain medications can increase the risk of GERD, including:
- NSAIDs (e.g., ibuprofen, aspirin): Can irritate the esophagus and stomach lining.
- Calcium Channel Blockers: Used for high blood pressure, can relax the LES.
- Anticholinergics: Used to treat conditions like allergies and asthma, can relax the LES.
- Benzodiazepines: Used for anxiety or insomnia, can relax the LES.
- Certain medications can increase the risk of GERD, including:
- Stress and Lack of Sleep:
- Stress doesn’t directly cause GERD, but it can contribute to behaviors (like overeating or smoking) that trigger reflux. Lack of sleep can also exacerbate GERD symptoms.
- Rapid Weight Gain:
- Sudden weight gain, even within a normal weight range, can increase the risk of GERD by increasing pressure on the abdomen.
GERD is a complex condition that often results from a combination of factors. Identifying and addressing these causes can help manage and reduce symptoms.
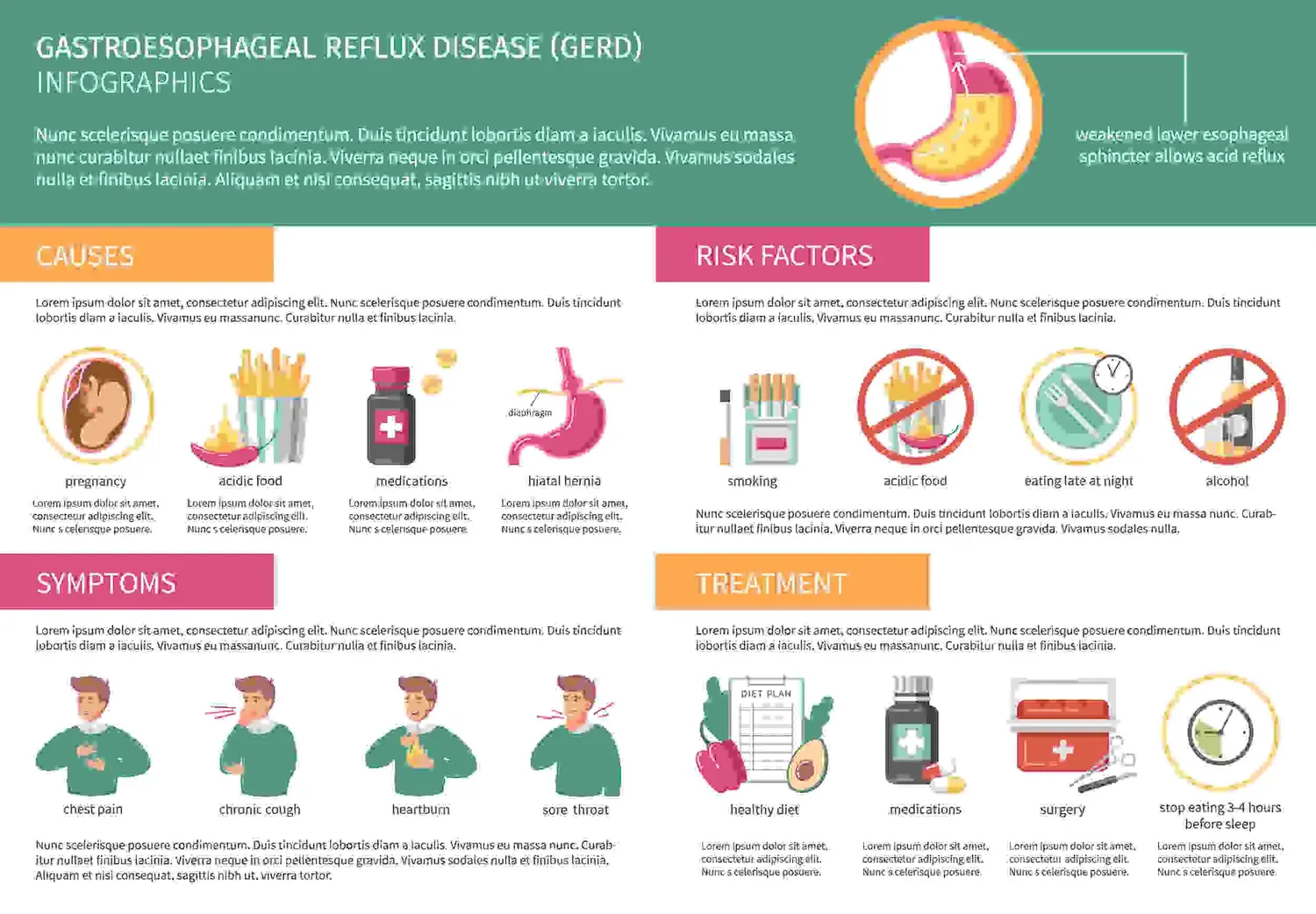
Symptoms
The symptoms of gastroesophageal reflux disease (GERD) can vary in severity and frequency, but the most common ones include:
Common Symptoms of GERD:
- Heartburn:
- A burning sensation in the chest, usually after eating, which might be worse at night or when lying down.
- Often feels like it’s rising from the stomach to the chest or even the throat.
- Regurgitation:
- The sensation of acid or food coming back up into the throat or mouth, sometimes leaving a sour or bitter taste.
- Dysphagia:
- Difficulty swallowing, feeling like food is stuck in the esophagus or throat.
- Chest Pain:
- Often mistaken for a heart attack, GERD-related chest pain typically feels like a burning or pressure in the chest, especially after eating.
- Chronic Cough:
- A persistent cough that is not related to respiratory conditions and often worsens at night or after eating.
- Hoarseness or Sore Throat:
- Acid reflux can irritate the vocal cords, leading to a hoarse voice or sore throat, especially in the morning.
- Lump in the Throat Sensation (Globus Sensation):
- A feeling of a lump in the throat that doesn’t go away with swallowing.
- Nausea or Vomiting:
- Some individuals with GERD may experience nausea, and in more severe cases, vomiting.
- Bloating and Burping:
- A sensation of fullness or bloating, and frequent belching, are sometimes associated with GERD.
- Bad Breath (Halitosis):
- Persistent bad breath, even with good oral hygiene, can be a sign of GERD.
Less Common Symptoms:
- Ear Pain: Sometimes, the acid reflux can cause referred pain in the ears.
- Asthma-Like Symptoms: GERD can exacerbate asthma symptoms or cause wheezing and shortness of breath.
- Chronic Sinusitis: Reflux may irritate the lining of the sinuses, leading to chronic sinus issues
complications
If left untreated, GERD (Gastroesophageal Reflux Disease) can lead to several serious complications. The chronic exposure of the esophagus to stomach acid can cause damage to the esophageal lining and result in a range of health issues.
Complications of GERD:
- Esophagitis:
- Inflammation of the Esophagus: Prolonged acid exposure can cause irritation and inflammation of the esophagus, leading to pain, discomfort, and difficulty swallowing.
- Esophageal Strictures:
- Narrowing of the Esophagus: Chronic inflammation can cause the formation of scar tissue, which narrows the esophagus and makes swallowing difficult. This condition is known as an esophageal stricture.
- Barrett’s Esophagus:
- Precancerous Changes: Long-term acid exposure can cause changes in the cells lining the lower esophagus. These cells can become more like the cells lining the intestines, a condition known as Barrett’s esophagus. While Barrett’s esophagus itself doesn’t cause symptoms, it increases the risk of developing esophageal cancer.
- Esophageal Ulcers:
- Open Sores in the Esophagus: The acid can wear away the lining of the esophagus, leading to the formation of painful ulcers that may bleed and cause difficulty swallowing.
- Esophageal Cancer:
- Adenocarcinoma of the Esophagus: Barrett’s esophagus increases the risk of developing adenocarcinoma, a type of esophageal cancer. This is a serious and potentially life-threatening complication.
- Chronic Cough and Laryngitis:
- Throat and Voice Box Issues: Acid reflux can irritate the throat and voice box (larynx), leading to a persistent cough, hoarseness, or chronic laryngitis.
- Aspiration Pneumonia:
- Lung Infections: Stomach acid can be aspirated (inhaled) into the lungs, leading to inflammation or infection, known as aspiration pneumonia.
- Dental Erosion:
- Tooth Decay: Acid reflux can cause the acid to reach the mouth, where it can erode tooth enamel, leading to tooth decay and sensitivity.
- Asthma Worsening:
- Respiratory Issues: GERD can exacerbate asthma symptoms or even trigger asthma in people who have never had it before. The exact connection isn’t fully understood, but it’s thought that acid reflux may irritate the airways and lungs.
- Sinus and Ear Infections:
- ENT Issues: Acid reflux can lead to chronic sinus infections and ear infections, as the acid can irritate the nasal passages and Eustachian tubes.
- Difficulty Swallowing (Dysphagia):
- Swallowing Issues: Complications like strictures or severe esophagitis can make it difficult or painful to swallow food or even liquids.
When to Seek Medical Attention:
If you experience severe or persistent GERD symptoms, or if you develop symptoms such as difficulty swallowing, unintentional weight loss, vomiting blood, or black stools, it’s important to seek medical attention immediately. These could be signs of serious complications that require prompt treatment.
Management
Management of gastroesophageal reflux disease (GERD) involves a combination of lifestyle modifications, medications, and in some cases, surgical interventions. The goal is to reduce symptoms, prevent complications, and improve the quality of life.
1. Lifestyle Modifications:
- Dietary Changes:
- Avoid Trigger Foods: Identify and avoid foods that trigger symptoms, such as spicy foods, fatty foods, chocolate, caffeine, alcohol, citrus, and tomato-based products.
- Eat Smaller, More Frequent Meals: Large meals can increase pressure on the LES, so smaller, more frequent meals are recommended.
- Avoid Eating Before Bed: Don’t eat at least 2-3 hours before lying down to reduce the risk of nighttime reflux.
- Weight Management:
- Lose Excess Weight: Obesity is a significant risk factor for GERD, so losing weight can help reduce symptoms.
- Elevate the Head of the Bed:
- Elevate Bed: Raise the head of the bed by 6-8 inches to prevent acid from flowing back into the esophagus during sleep.
- Quit Smoking:
- Stop Smoking: Smoking weakens the LES and increases acid production, so quitting is essential.
- Avoid Tight Clothing:
- Wear Loose Clothing: Avoid tight belts and clothing around the waist, as they can increase pressure on the abdomen and LES.
- Posture Adjustments:
- Stay Upright After Meals: Sit upright for at least 2-3 hours after eating to help prevent reflux.
2. Medications:
- Over-the-Counter (OTC) Medications:
- Antacids: Neutralize stomach acid and provide quick, short-term relief (e.g., Tums, Rolaids, Mylanta).
- H2 Blockers: Reduce acid production and are effective for mild to moderate symptoms (e.g., ranitidine, famotidine).
- Prescription Medications:
- Proton Pump Inhibitors (PPIs): These are the most effective medications for reducing stomach acid and healing the esophagus (e.g., omeprazole, esomeprazole, lansoprazole). They are typically used for more severe GERD or when symptoms are not controlled by H2 blockers.
- Prokinetics: Help strengthen the LES and speed up gastric emptying (e.g., metoclopramide). They are used less frequently due to side effects.
- Baclofen: Reduces the frequency of transient LES relaxations, though it may have side effects like fatigue.
- Alginate-Based Formulations:
- Gaviscon: Forms a protective barrier on top of the stomach contents, reducing the risk of reflux.
3. Surgical and Endoscopic Interventions:
- Nissen Fundoplication:
- Surgical Option: In this procedure, the top part of the stomach is wrapped around the LES to strengthen it and prevent reflux. This is usually recommended for patients who do not respond to medications or prefer a long-term solution.
- Laparoscopic Procedures:
- Minimally Invasive Surgery: Techniques like laparoscopic fundoplication offer a less invasive surgical option with shorter recovery times.
- LINX Device:
- Magnetic Sphincter Augmentation: A ring of magnetic beads is placed around the LES to strengthen it while allowing food to pass through. This is a newer, minimally invasive procedure.
- Endoscopic Therapies:
- Stretta Procedure: Radiofrequency energy is used to tighten the LES.
- Endoscopic Fundoplication: A less invasive alternative to traditional fundoplication, where part of the stomach is folded and sewn to reinforce the LES.
4. Monitoring and Follow-Up:
- Regular Monitoring: Patients with chronic or severe GERD should be monitored for complications such as Barrett’s esophagus, especially if symptoms persist despite treatment.
- Endoscopy: This may be recommended for patients with alarming symptoms (e.g., difficulty swallowing, weight loss, anemia) or to assess the severity of esophageal damage.
5. Alternative and Complementary Therapies:
- Herbal Remedies: Some patients find relief with herbal remedies like licorice root (DGL) or slippery elm, although these should be used with caution and under the guidance of a healthcare provider.
- Acupuncture: Some evidence suggests acupuncture may help reduce GERD symptoms, though it is not a primary treatment.
6. Education and Patient Support:
- Patient Education: Understanding the condition and how to manage triggers is crucial. Patients should be informed about the importance of adherence to lifestyle changes and medication regimens.
- Support Groups: Participation in support groups can help patients cope with the chronic nature of GERD.
7. Managing Complications:
- Barrett’s Esophagus: Patients with this condition require regular surveillance endoscopy to monitor for dysplasia or early signs of cancer.
- Strictures: Esophageal dilation may be needed to treat strictures caused by chronic acid exposure.
Conclusion
In conclusion, gastroesophageal reflux disease (GERD) is a common yet potentially serious condition that results from the backward flow of stomach acid into the esophagus, leading to symptoms like heartburn, regurgitation, and discomfort. The pathophysiology of GERD involves multiple factors, including a weakened lower esophageal sphincter (LES), delayed gastric emptying, and increased intra-abdominal pressure.
Effective management of GERD requires a comprehensive approach that includes lifestyle modifications, dietary changes, and medications such as antacids, H2 blockers, and proton pump inhibitors. For those with severe or refractory GERD, surgical and endoscopic interventions may be necessary. Regular monitoring and follow-up are essential to prevent complications such as esophagitis, Barrett’s esophagus, and esophageal cancer.
By adhering to a tailored treatment plan and making appropriate lifestyle adjustments, most patients can achieve significant symptom relief and reduce the risk of long-term complications. Early recognition and intervention are key to managing GERD effectively and maintaining overall well-being.
Disclaimer: This information provides a general overview of diagnosis, treatment, and medication related to alopecia areata. It is intended to assist in understanding potential options but is not comprehensive. This content is not a substitute for professional medical advice, diagnosis, or treatment. It does not cover all possible conditions, treatments, side effects, or risks specific to individual cases. For personalized medical advice, please consult a healthcare provider who can evaluate your unique circumstances. This information does not endorse or validate any specific treatments or medications.
Faqs
Can GERD cause back pain?
Yes, GERD can cause back pain, particularly in the upper back, due to referred pain from the esophagus or muscle strain from poor posture related to reflux symptoms.
Can people with GERD eat cherries?
People with GERD should be cautious with cherries, as their acidity may trigger reflux symptoms in some individuals. However, they can be eaten in moderation if they do not cause discomfort.
What is the relation between coffee and GERD?
Coffee can worsen GERD symptoms by relaxing the lower esophageal sphincter and increasing stomach acid production, making it a common trigger for acid reflux.
Can GERD lead to cancer ?
Yes, untreated GERD can lead to a condition called Barrett's esophagus, which increases the risk of developing esophageal cancer.
How to stop GERD cough instantly?
To stop a GERD-related cough instantly, try sipping water, chewing gum to increase saliva production, or taking an antacid to neutralize stomach acid. However, managing GERD long-term is key to reducing the cough.
Is GERD genetic ?
Yes, GERD can have a genetic component, making it more likely to occur in individuals with a family history of the condition.
Is probiotics good for GERD?
Probiotics may help improve GERD symptoms by balancing gut bacteria and reducing inflammation, but they are not a cure. They can be a useful supplement to other GERD treatments.




