Understanding Anemia: Causes, Symptoms, and Treatment
Introduction
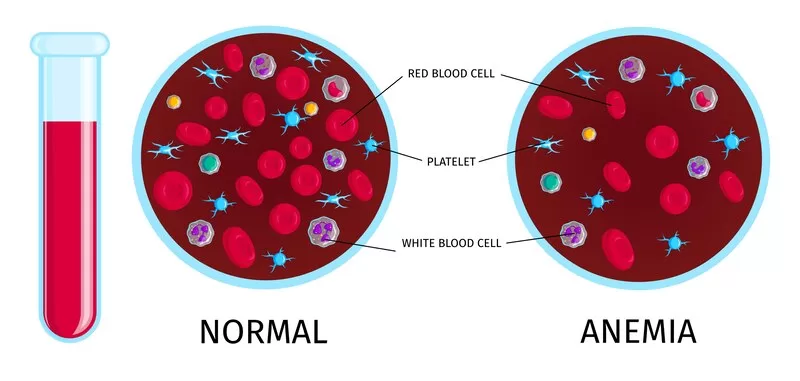
Anemia is a common blood disorder affecting millions of people worldwide. It occurs when the body doesn’t have enough healthy red blood cells to carry adequate oxygen to tissues. This can lead to fatigue, weakness, and a variety of other health issues. In this blog, we will explore the different types of anemia, their causes, symptoms, and available treatments.
Types:
Anemia is a condition characterized by a deficiency of red blood cells or hemoglobin, which leads to reduced oxygen delivery to the body’s tissues. There are several types of anemia, each with unique causes, symptoms, and treatment options. Here’s an in-depth look at the most common types:
1. Iron-Deficiency Anemia
Cause: Iron-deficiency anaemia is the most common type and is caused by a lack of iron in the body. Iron is essential for producing hemoglobin, the protein in red blood cells that carries oxygen.
Risk Factors:
- Poor diet lacking in iron-rich foods
- Blood loss from heavy menstrual periods or internal bleeding (e.g., ulcers, colon cancer)
- Inability to absorb iron (e.g., celiac disease, gastric bypass surgery)
Symptoms:
- Fatigue and weakness
- Pale skin
- Shortness of breath
- Dizziness
- Cold hands and feet
- Brittle nails
2. Vitamin Deficiency Anemia
Cause: This type is caused by a lack of essential vitamins needed for red blood cell production, primarily vitamin B12 and folate.
Risk Factors:
- Poor dietary intake of B12 and folate
- Conditions affecting absorption (e.g., pernicious anemia, Crohn’s disease)
- Pregnancy, which increases folate requirements
Symptoms:
- Fatigue and weakness
- Pale or yellowish skin
- Heart palpitations
- Shortness of breath
- Neurological issues (e.g., numbness, tingling, balance problems)
- Memory difficulties
3. Aplastic Anemia
Cause: It is a rare but serious condition where the bone marrow fails to produce enough blood cells, including red blood cells.
Risk Factors:
- Exposure to toxic chemicals (e.g., benzene)
- Certain medications
- Autoimmune disorders
- Viral infections (e.g., hepatitis, Epstein-Barr virus)
- Radiation and chemotherapy
Symptoms:
- Fatigue and weakness
- Frequent infections
- Rapid heart rate
- Unexplained or easy bruising and bleeding
- Shortness of breath
4. Hemolytic Anemia
Cause: It occurs when red blood cells are destroyed faster than they can be produced.
Risk Factors:
- Genetic disorders (e.g., sickle cell disease, thalassemia)
- Autoimmune conditions
- Infections
- Certain medications
- Blood transfusion reactions
Symptoms:
- Fatigue and weakness
- Shortness of breath
- Jaundice (yellowing of the skin and eyes)
- Dark urine
- Enlarged spleen
- Rapid heart rate
5. Sickle Cell Anemia
Cause: Sickle cell disease is a genetic disorder where red blood cells are abnormally shaped like crescents or sickles. These cells can block blood flow and break down prematurely.
Risk Factors:
- Inherited from both parents carrying the sickle cell trait
Symptoms:
- Painful episodes (crises)
- Fatigue
- Swelling in hands and feet
- Frequent infections
- Delayed growth in children
- Vision problems
6. Thalassemia
Cause: Thalassemia is a group of inherited blood disorders characterized by the body making an abnormal form of hemoglobin, leading to excessive destruction of red blood cells.
Risk Factors:
- Family history of thalassemia
- Certain ethnic backgrounds (Mediterranean, South Asian, African)
Symptoms:
- Mild to severe anemia
- Fatigue and weakness
- Pale or yellowish skin
- Facial bone deformities
- Slow growth
- Abdominal swelling
Causes:
Anemia occurs when the body does not have enough healthy red blood cells to carry adequate oxygen to tissues. This can be due to a variety of underlying causes, each contributing to different types of anemia. Here’s a detailed look at the primary causes:
1. Iron-Deficiency Anemia
Iron-deficiency anemia is the most common type of anemia and occurs due to insufficient iron, which is essential for hemoglobin production.
Causes:
- Inadequate Dietary Intake: Diets low in iron-rich foods such as meat, beans, lentils, and fortified cereals.
- Blood Loss: Chronic blood loss from heavy menstrual periods, gastrointestinal bleeding (e.g., ulcers, colon cancer, hemorrhoids), or frequent blood donations.
- Poor Absorption: Conditions that affect the absorption of iron from the digestive tract, such as celiac disease, Crohn’s disease, or gastric bypass surgery.
- Increased Needs: Pregnancy, breastfeeding, or periods of rapid growth in children and adolescents.
2. Vitamin Deficiency Anemia
Vitamin deficiency anemia occurs due to a lack of vitamins needed for red blood cell production, particularly vitamin B12 and folate.
Causes:
- Inadequate Dietary Intake: Diets lacking in vitamin B12 (found in meat, dairy, and eggs) or folate (found in leafy green vegetables, fruits, and fortified cereals).
- Absorption Issues: Conditions such as pernicious anemia, which affects vitamin B12 absorption, and other gastrointestinal disorders like Crohn’s disease and celiac disease.
- Increased Needs: Pregnancy increases the need for folate to support fetal development.
- Alcoholism: Excessive alcohol consumption can interfere with the absorption and metabolism of folate.
3. Aplastic Anemia
Aplastic anemia is a rare and serious condition where the bone marrow fails to produce enough new blood cells.
Causes:
- Autoimmune Disorders: Conditions where the immune system attacks the bone marrow.
- Toxic Exposure: Exposure to chemicals such as benzene, pesticides, and certain medications (e.g., chemotherapy drugs).
- Radiation Therapy: High doses of radiation used to treat cancers.
- Infections: Viral infections such as hepatitis, Epstein-Barr virus, and HIV.
- Genetic Disorders: Conditions like Fanconi anemia.
4. Hemolytic Anemia
Hemolytic anemia occurs when red blood cells are destroyed faster than they can be produced.
Causes:
- Inherited Conditions: Genetic disorders such as sickle cell disease and thalassemia.
- Autoimmune Reactions: Conditions where the immune system mistakenly attacks and destroys red blood cells (e.g., autoimmune hemolytic anemia).
- Infections: Certain infections can lead to the destruction of red blood cells.
- Medications: Some drugs can trigger hemolysis, including certain antibiotics and anti-malarial medications.
- Blood Transfusion Reactions: Receiving a blood transfusion with incompatible blood type.
5. Sickle Cell Anemia
Sickle cell anemia is a genetic disorder where red blood cells become abnormally shaped, leading to blockages in blood flow and premature cell death.
Causes:
- Genetic Mutation: Inherited from both parents who carry the sickle cell trait. The abnormal hemoglobin (hemoglobin S) causes red blood cells to become rigid and shaped like a sickle.
6. Thalassemia
Thalassemia is a group of inherited blood disorders characterized by abnormal hemoglobin production, leading to the destruction of red blood cells.
Causes:
- Genetic Mutations: Inherited mutations that affect hemoglobin production. There are different types, including alpha-thalassemia and beta-thalassemia, depending on which part of the hemoglobin molecule is affected.
7. Chronic Disease Anemia
Chronic disease anemia is associated with chronic conditions that interfere with red blood cell production.
Causes:
- Chronic Kidney Disease: Reduced erythropoietin production, a hormone necessary for red blood cell production.
- Chronic Infections and Inflammatory Diseases: Conditions like rheumatoid arthritis, lupus, and inflammatory bowel disease.
- Cancer: Some cancers and cancer treatments can affect bone marrow function and red blood cell production.
8. Bone Marrow Disorders
Bone marrow disorders can lead to anemia by affecting the production of blood cells.
Causes:
- Leukemia: Cancer of the blood and bone marrow.
- Myelodysplastic Syndromes: Disorders caused by poorly formed or dysfunctional blood cells.
- Multiple Myeloma: Cancer of plasma cells in the bone marrow.
Diagnosis of Anemia:
Diagnosing anaemia involves a systematic approach that includes medical history, physical examination, and various laboratory tests to determine the type and cause of anaemia. Here’s an in-depth look at the diagnostic process for anemia:
1. Medical History
The diagnostic process begins with a detailed medical history. Your healthcare provider will ask about:
- Symptoms: Fatigue, weakness, shortness of breath, dizziness, paleness, and other related symptoms.
- Dietary Habits: To identify potential deficiencies in iron, vitamin B12, or folate.
- Menstrual History: In women, heavy menstrual bleeding can be a significant cause of iron-deficiency anemia.
- Family History: Any family members with anemia or related genetic conditions like sickle cell disease or thalassemia.
- Chronic Conditions: Presence of chronic diseases such as kidney disease, cancer, or autoimmune disorders.
- Medications: Any medications that might affect blood cell production or cause bleeding.
2. Physical Examination
A physical examination helps to identify signs that may suggest anemia or its underlying causes:
- Pale Skin and Mucous Membranes: Indicating low hemoglobin levels.
- Rapid or Irregular Heartbeat: Anemia can cause the heart to work harder to deliver oxygen.
- Swollen or Tender Lymph Nodes: May suggest an infection or cancer.
- Enlarged Spleen or Liver: Can indicate hemolytic anemia or other underlying conditions.
- Neurological Signs: Numbness or tingling may suggest vitamin B12 deficiency.
3. Laboratory Tests
Several blood tests are essential for diagnosing anemia and determining its type and cause:
- Complete Blood Count (CBC):
- Hemoglobin (Hb): Measures the amount of hemoglobin in the blood. Low levels indicate anaemia.
- Hematocrit (Hct): The proportion of red blood cells in the blood. Low hematocrit is a sign of anaemia.
- Red Blood Cell Count (RBC): The number of red blood cells in the blood. A low count suggests anaemia.
- Mean Corpuscular Volume (MCV): Measures the average size of red blood cells. Helps classify anaemia as microcytic (small cells), normocytic (normal-sized cells), or macrocytic (large cells).
- Mean Corpuscular Hemoglobin (MCH): MCH measures the average amount of hemoglobin in a single red blood cell. Low MCH can indicate microcytic anaemia; high MCH can indicate macrocytic anaemia.
- Mean Corpuscular Hemoglobin Concentration (MCHC): MCHC measures the average concentration of hemoglobin in red blood cells. Low MCHC suggests hypochromic anemia (cells have less color, often seen in iron deficiency anemia).
- Red Cell Distribution Width (RDW): RDW indicates the variation in the size of red blood cells. High RDW indicates a significant variation in red blood cell size, which can be seen in various types of anemia.
- Iron Studies:
- Serum Iron: The amount of iron in the blood.
- Ferritin: Indicates the amount of stored iron in the body. Low levels suggest iron-deficiency.
- Total Iron-Binding Capacity (TIBC): Measures the blood’s capacity to bind iron with transferrin. Elevated TIBC indicates iron deficiency.
- Transferrin Saturation: The percentage of transferrin that is saturated with iron. Low saturation suggests iron-deficiency.
- Vitamin Levels:
- Vitamin B12: Low levels indicate vitamin B12 deficiency anemia.
- Folate (Vitamin B9): Low levels suggest folate deficiency anemia.
- Reticulocyte Count:
- Measures the number of young red blood cells in the blood. A high count can indicate hemolytic anemia or blood loss, while a low count can suggest bone marrow problems.
- Peripheral Blood Smear:
- Examines the shape and appearance of red blood cells under a microscope. Abnormal shapes can help diagnose specific types of anemia, such as sickle cell anemia or thalassemia.
- Bone Marrow Biopsy and Aspiration:
- Performed if a bone marrow disorder is suspected. It involves extracting a small sample of bone marrow to examine the production of blood cells.
- Additional Tests:
- Electrophoresis: Used to diagnose hemoglobinopathies like sickle cell disease and thalassemia by identifying abnormal hemoglobin types.
- Liver Function Tests: To check for liver diseases that might cause anaemia.
- Kidney Function Tests: To assess for chronic kidney disease, which can lead to anaemia.
4. Differential Diagnosis
It’s important to differentiate anemia from other conditions that may present with similar symptoms. The healthcare provider will consider:
- Chronic Diseases: Conditions like chronic kidney disease, cancer, and autoimmune disorders.
- Infections: Chronic infections that can lead to anemia of chronic disease.
- Medications: Drugs that can cause bone marrow suppression or hemolysis.
- Nutritional Deficiencies: Ensuring that dietary causes of anemia are accurately identified and treated.
Management:
Managing anemia involves addressing the underlying cause, alleviating symptoms, and restoring normal red blood cell levels and function. Here’s an in-depth guide to the management of various types of anaemia:
1. Iron-Deficiency Anemia
Treatment Goals:
- Replenish iron stores
- Address the cause of iron loss
Management Strategies:
- Oral Iron Supplements: Ferrous sulfate, ferrous gluconate, or ferrous fumarate are commonly prescribed. These should be taken on an empty stomach for better absorption but can be taken with food if they cause stomach upset.
- Dietary Changes: Increase intake of iron-rich foods such as red meat, poultry, fish, lentils, beans, spinach, and iron-fortified cereals. Vitamin C-rich foods (e.g., citrus fruits, tomatoes) can enhance iron absorption.
- Treat Underlying Causes: Address sources of chronic blood loss, such as heavy menstrual periods (possibly with hormonal treatments) or gastrointestinal bleeding (with medications or surgery).
Monitoring:
- Regular follow-up blood tests to monitor hemoglobin levels and iron stores.
2. Vitamin B12 Deficiency Anemia
Treatment Goals:
- Correct vitamin B12 deficiency
- Prevent neurological complications
Management Strategies:
- Vitamin B12 Injections: Initial treatment often involves frequent injections (daily or weekly) followed by monthly maintenance injections.
- Oral or Sublingual Supplements: High-dose oral B12 supplements may be effective for some patients.
- Dietary Adjustments: Include more B12-rich foods in the diet, such as meat, dairy products, eggs, and fortified cereals.
Monitoring:
- Regular blood tests to ensure normal B12 levels and resolution of anemia symptoms.
3. Folate Deficiency Anemia
Treatment Goals:
- Restore normal folate levels
- Address the underlying cause of deficiency
Management Strategies:
- Oral Folate Supplements: Usually taken daily until levels are normalized.
- Dietary Changes: Increase intake of folate-rich foods such as leafy green vegetables, citrus fruits, beans, and fortified cereals.
- Treat Underlying Causes: Address factors contributing to folate deficiency, such as excessive alcohol consumption or certain medications.
Monitoring:
- Follow-up blood tests to monitor folate levels and anemia resolution.
4. Aplastic Anemia
Treatment Goals:
- Stimulate bone marrow to produce blood cells
- Address the underlying cause or trigger
Management Strategies:
- Immunosuppressive Therapy: Drugs such as anti thymocyte globulin (ATG) and cyclosporine to suppress the immune system and allow bone marrow recovery.
- Bone Marrow Transplant: Potentially curative for some patients, especially younger ones with a suitable donor.
- Blood Transfusions: To manage severe anaemia and other blood cell deficiencies.
- Growth Factors: Medications like erythropoietin or granulocyte-colony stimulating factor (G-CSF) to stimulate blood cell production.
Monitoring:
- Regular blood counts and monitoring for complications or response to therapy.
5. Hemolytic Anemia
Treatment Goals:
- Reduce red blood cell destruction
- Treat underlying causes
Management Strategies:
- Corticosteroids: To reduce immune-mediated red blood cell destruction.
- Immunosuppressive Drugs: In cases where corticosteroids are ineffective or inappropriate.
- Blood Transfusions: To maintain adequate red blood cell levels in severe cases.
- Splenectomy: Surgical removal of the spleen in cases of severe, refractory hemolytic anemia.
Monitoring:
- Regular blood counts and monitoring for hemolysis markers and treatment efficacy.
6. Sickle Cell Anemia
Treatment Goals:
- Manage pain and prevent complications
- Improve quality of life
Management Strategies:
- Pain Management: Use of pain relief medications and hydration during sickle cell crises.
- Hydroxyurea: A medication that reduces the frequency of pain episodes and the need for blood transfusions.
- Blood Transfusions: To treat severe anemia and prevent complications like stroke.
- Bone Marrow Transplant: Potentially curative but associated with significant risks.
Monitoring:
- Regular follow-ups to manage complications and monitor treatment response.
7. Thalassemia
Treatment Goals:
- Maintain adequate hemoglobin levels
- Prevent iron overload
Management Strategies:
- Regular Blood Transfusions: To maintain hemoglobin levels.
- Iron Chelation Therapy: Medications like deferoxamine, deferasirox, or deferiprone to remove excess iron from the body.
- Bone Marrow Transplant: Can be curative in some cases, especially in children with a matched donor.
Monitoring:
- Regular blood tests to monitor iron levels and organ function.
Preventing Anemia
Some types of anemia can be prevented with lifestyle changes and dietary adjustments:
- Balanced Diet: Ensure a diet rich in iron, vitamin B12, and folate.
- Regular Check-Ups: Monitor for chronic diseases that can cause anaemia.
- Supplements: Take iron and vitamin supplements if needed, especially for pregnant women and those with dietary restrictions.
Anemia Care Plan
Creating a care plan for anemia involves addressing the underlying causes and managing symptoms effectively. Here’s a structured approach:
Assessment and Diagnosis
- Medical History and Physical Examination:
- Gather information about the patient’s symptoms, medical history, medications, and any recent surgeries or illnesses.
- Conduct a thorough physical examination to assess for signs of anemia and its potential causes.
- Diagnostic Tests:
- Perform blood tests to confirm the diagnosis of anemia, determine the type (e.g., iron-deficiency anemia, vitamin B12 deficiency anemia), and assess the severity.
- Additional tests may include iron studies, vitamin B12 and folate levels, reticulocyte count, and peripheral blood smear.
Treatment Goals
- Correcting Underlying Causes:
- Identify and treat the underlying cause of anemia, such as iron deficiency, vitamin deficiency, chronic disease, or blood loss.
- Address any dietary deficiencies through nutrition counseling and supplementation as needed.
- Symptom Management:
- Manage symptoms such as fatigue, weakness, dizziness, and shortness of breath.
- Provide supportive care, including rest and assistance with activities of daily living if needed.
Care Plan Interventions
- Nutritional Support:
- Recommend a diet rich in iron, vitamin B12, folate, and other nutrients essential for red blood cell production.
- Consider supplements if dietary intake is inadequate or malabsorption is suspected.
- Medication Therapy:
- Prescribe iron supplements, vitamin B12 injections or oral supplements, or erythropoiesis-stimulating agents (ESA) in cases of chronic kidney disease or chemotherapy-induced anemia.
- Monitor for medication adherence, side effects, and therapeutic response.
- Monitoring and Follow-Up:
- Schedule regular follow-up visits to monitor hemoglobin levels, iron status, and response to treatment.
- Adjust treatment plan based on clinical response and diagnostic tests.
- Patient Education:
- Educate the patient and family members about the importance of compliance with medications, dietary modifications, and lifestyle changes.
- Discuss signs and symptoms of worsening anemia or potential complications requiring immediate medical attention.
Referral and Collaborative Care
- Consultation and Referral:
- Consider referral to a hematologist or specialist if further evaluation or management is needed, such as in cases of refractory anemia or suspected underlying hematologic disorders.
- Multidisciplinary Approach:
- Collaborate with dietitians, pharmacists, social workers, and other healthcare professionals to provide comprehensive care and support for the patient.
Goals of Care
- Achieve and Maintain Hemoglobin Levels:
- Aim to restore hemoglobin levels to normal or target ranges based on individual patient factors and underlying conditions.
- Prevent recurrence of anemia through ongoing management and monitoring.
- Improve Quality of Life:
- Reduce symptoms of anemia, enhance functional capacity, and improve overall well-being and quality of life for the patient.
By implementing a structured care plan tailored to the individual needs and circumstances of the patient, healthcare providers can effectively manage anemia, address underlying causes, and optimize outcomes. Regular reassessment and adjustments to the plan are essential to ensure ongoing care and support.
Conclusion
Anaemia is a common condition with a variety of causes and manifestations. Understanding the different types, recognizing symptoms, and seeking appropriate treatment are crucial steps in managing this condition effectively. With proper care, most people with anaemia can lead healthy and active lives. If you suspect you have anaemia, consult a healthcare professional for a thorough evaluation and tailored treatment plan.
FAQs,
Can a white person have sickle cell anemia?
Yes, a white person can have sickle cell disease, although it is more common among people of African, Mediterranean, Middle Eastern, and Indian ancestry. Sickle cell anemia is a genetic disorder caused by a mutation in the hemoglobin gene. Anyone with two copies of the mutated gene (one from each parent) can develop the disease, regardless of their racial or ethnic background. While the prevalence is higher in certain populations, it is not exclusive to them.
Can anemia cause high blood pressure?
Anaemia and high blood pressure are generally distinct conditions, but they can be related in certain circumstances. Chronic Kidney Disease: Anaemia is common in people with chronic kidney disease (CKD), which can also cause high blood pressure. Damaged kidneys produce less erythropoietin, leading to anemia, and are less effective at regulating blood pressure. Heart Conditions: Severe anemia can lead to increased cardiac output as the heart works harder to supply oxygen to the body. Over time, this increased workload can contribute to high blood pressure. Iron-Deficiency Anemia and Pulmonary Hypertension: While not common, iron-deficiency anemia can be associated with pulmonary hypertension, which is high blood pressure in the arteries of the lungs. In most cases, anemia itself does not directly cause high blood pressure, but the underlying health conditions that lead to anemia might also contribute to elevated blood pressure.
How to treat anemia in dogs at home?
Treating anaemia in dogs at home should be done under the guidance of a veterinarian, as anaemia can be a sign of various underlying health issues. However, some supportive measures can be taken to help manage the condition alongside veterinary care: Nutritious Diet: Provide a balanced diet rich in iron, vitamins, and minerals. Consider dog foods formulated for dogs with anemia or consult with your vet about appropriate dietary supplements. Iron-Rich Foods: Incorporate iron-rich foods such as lean meats (beef, chicken, liver), fish, and eggs into your dog's diet. Ensure these foods are cooked and appropriate for canine consumption. Vitamin Supplements: Supplements with vitamins B12, B6, and C can help improve iron absorption and red blood cell production. Consult your vet before starting any supplements. Hydration: Ensure your dog stays well-hydrated, as dehydration can worsen anemia symptoms. Avoid Toxins: Keep your dog away from substances that can cause anemia, such as certain plants, medications, or foods that are toxic to dogs (e.g., onions, garlic, chocolate). Rest: Ensure your dog gets plenty of rest and avoids strenuous activities to reduce the strain on their body. It's essential to work closely with a veterinarian to identify and treat the underlying cause of the anemia.
Does hemoglobin drop during your period?
Yes, hemoglobin levels can drop slightly during menstruation due to the loss of blood. However, the extent of the drop depends on the amount of blood lost during the menstrual period. Blood Loss Volume: The average menstrual blood loss is about 30-40 milliliters, which usually has a minimal impact on hemoglobin levels. Women with heavy menstrual bleeding (menorrhagia) can lose significantly more blood, which can have a more noticeable effect on hemoglobin levels. Iron Stores: Women with adequate iron stores and a well-balanced diet are better able to compensate for the blood loss, maintaining stable hemoglobin levels. Women with low iron stores or poor dietary iron intake are at higher risk of a significant drop in hemoglobin during menstruation.
Can anemia cause depression?
Yes, anemia can cause depression. The reduced oxygen supply to the brain, fatigue, and nutritional deficiencies associated with anemia can contribute to depressive symptoms.
Why does anaemia cause heart failure?
Anaemia can cause heart failure due to the following reasons: Increased Cardiac Output: To compensate for the reduced oxygen-carrying capacity of the blood, the heart pumps more blood to deliver sufficient oxygen to tissues. This increased workload can strain the heart over time. Tachycardia: Anaemia often leads to a faster heart rate (tachycardia) as the body tries to compensate for the reduced oxygen delivery. Persistent tachycardia can weaken the heart muscle. Left Ventricular Hypertrophy: The increased demand on the heart can cause the left ventricle to thicken (hypertrophy). This adaptation initially helps maintain cardiac output but eventually leads to stiffness and impaired function. Increased Blood Volume: Chronic anaemia can lead to an increase in plasma volume to maintain blood pressure and perfusion. This extra volume further increases the workload on the heart. Reduced Oxygen Supply to Heart Tissue: The heart itself may receive less oxygen due to anemia, impairing its function and contributing to the development of heart failure. Over time, these compensatory mechanisms can lead to the heart becoming enlarged and weakened, eventually resulting in heart failure.