Introduction
Uterine fibroids, also known as leiomyomas or myomas, are non-cancerous growths that develop in or around the uterus. While often asymptomatic, fibroids can lead to significant health issues, including heavy menstrual bleeding, pelvic pain, and fertility challenges. With advancements in medical research, treatment options have evolved, offering more effective and less invasive ways to manage this common condition.
What Are Uterine Fibroids?
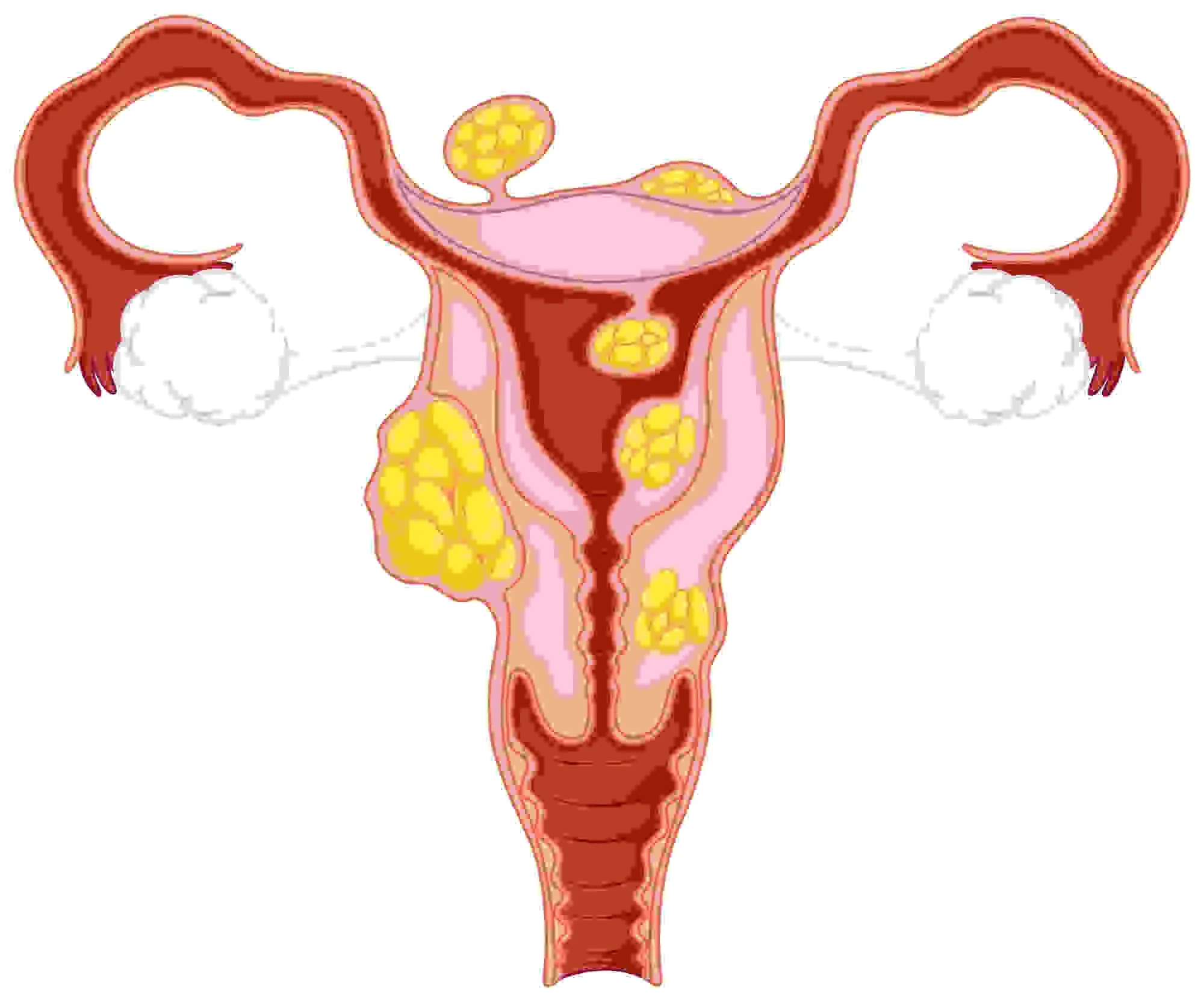
Uterine fibroids are benign tumors made up of muscle and connective tissue from the uterine wall. They can vary in size, from as small as a seed to as large as a melon, and can be single or multiple. Fibroids are classified based on their location in the uterus:
1. Intramural Fibroids
- Location: These uterine fibroids develop within the muscular wall (myometrium) of the uterus.
- Characteristics: They are the most common type of fibroid and can cause the uterus to appear larger than normal.
- Symptoms: Often associated with heavy menstrual bleeding, pelvic pain, and pressure on surrounding organs.
2. Subserosal Fibroids
- Location: These uterine fibroids grow on the outer surface of the uterus, beneath the serosa (the outermost layer of the uterus).
- Characteristics: They can grow large and extend outward, sometimes attaching to surrounding organs.
- Symptoms: May cause pressure symptoms, such as frequent urination or constipation, but are less likely to affect menstrual flow.
3. Submucosal Fibroids
- Location: These uterine fibroids develop just beneath the lining of the uterine cavity (endometrium).
- Characteristics: They are less common but can grow into the uterine cavity, distorting its shape.
- Symptoms: Often lead to severe menstrual bleeding, prolonged periods, and can be associated with infertility or pregnancy complications.
4. Pedunculated Fibroids
- Location: These uterine fibroids are attached to the uterine wall by a thin stalk, either inside the uterine cavity (pedunculated submucosal) or on the outside of the uterus (pedunculated subserosal).
- Characteristics: They can move or twist, causing severe pain.
- Symptoms: Depending on their location, they can cause similar symptoms to subserosal or submucosal fibroids, including pain and pressure.
5. Cervical Fibroids
- Location: These uterine fibroids develop in the cervical tissue, the lower part of the uterus that connects to the vagina.
- Characteristics: Less common than other types of fibroids.
- Symptoms: Can cause issues with urination, sexual intercourse, and abnormal bleeding.
6. Intracavitary Fibroids
- Location: These uterine fibroids are located within the uterine cavity.
- Characteristics: A subset of submucosal fibroids, they can be more problematic due to their position inside the cavity.
- Symptoms: Often linked to heavy menstrual bleeding, spotting between periods, and fertility issues.
Understanding the type of fibroid is crucial for determining the best treatment options, as different types can cause varying symptoms and complications.
Symptoms of Uterine Fibroids
Uterine fibroids can cause a variety of symptoms, depending on their size, number, and location. However, many women with fibroids experience no symptoms at all. When symptoms do occur, they can range from mild to severe and may include the following:
1. Heavy or Prolonged Menstrual Bleeding
- Menorrhagia: This is the most common symptom of fibroids. Women may experience unusually heavy or prolonged menstrual periods, sometimes with large blood clots. This can lead to anemia (low red blood cell count), causing fatigue and weakness.
2. Pelvic Pain and Pressure
- Pelvic Discomfort: Fibroids can cause a sense of fullness or pressure in the lower abdomen or pelvis, similar to the feeling of being pregnant.
- Lower Back Pain: Some women experience pain in the lower back, which can be constant or related to the menstrual cycle.
- Pain During Intercourse (Dyspareunia): Fibroids located near the cervix or in the lower part of the uterus can cause pain during sexual intercourse.
3. Frequent Urination or Urinary Retention
- Bladder Pressure: Large fibroids can press against the bladder, leading to a frequent need to urinate or difficulty in completely emptying the bladder.
4. Constipation
- Bowel Pressure: Fibroids, especially large subserosal ones, can press against the rectum, leading to constipation or difficulty with bowel movements.
5. Abdominal Swelling
- Enlarged Abdomen: Large fibroids can cause the abdomen to swell, making a woman appear pregnant or causing discomfort due to the pressure.
6. Reproductive Issues
- Infertility: Fibroids, particularly submucosal types, can interfere with the implantation of an embryo, leading to difficulties in conceiving.
- Recurrent Miscarriages: Fibroids can increase the risk of miscarriage, particularly if they distort the uterine cavity or affect the blood flow to a developing embryo.
- Complications During Pregnancy: Fibroids can cause complications such as preterm birth, breech position, or the need for a cesarean section.
7. Menstrual Irregularities
- Spotting or Bleeding Between Periods: Some women with fibroids experience irregular bleeding or spotting between menstrual periods.
8. Anemia
- Fatigue and Weakness: Due to heavy menstrual bleeding, women with fibroids are at risk of developing anemia, which can cause symptoms like fatigue, weakness, and shortness of breath.
9. Painful Menstruation (Dysmenorrhea)
- Cramping: Some women experience severe menstrual cramps, which may be more intense if fibroids are present.
10. Leg Pain
- Sciatica-Like Symptoms: In rare cases, large fibroids can press on nerves in the pelvis, causing pain that radiates down the leg, similar to sciatica.
Causes and Risk Factors
The exact cause of uterine fibroids is not fully understood, but several factors are believed to contribute to their development. Here’s a look at the primary causes and risk factors associated with uterine fibroids:
Causes of Uterine Fibroids
- Hormonal Factors
- Estrogen and Progesterone: These two hormones, which regulate the menstrual cycle, are thought to promote the growth of fibroids. Fibroids contain more estrogen and progesterone receptors than normal uterine muscle cells, which may explain why they grow during the reproductive years when hormone levels are highest. After menopause, when hormone levels decrease, fibroids often shrink.
- Genetic Changes
- Genetic Mutations: Many fibroids contain genetic alterations that are different from those in normal uterine muscle cells. For example, mutations in genes related to cell growth and replication can contribute to the development of fibroids.
- Growth Factors
- Insulin-like Growth Factors (IGFs): These proteins are involved in cell growth and development and may play a role in fibroid growth. An increased level of certain growth factors can stimulate fibroid formation and enlargement.
- Extracellular Matrix (ECM)
- Structural Support: The ECM, which provides structural support to cells, is often increased in fibroids. This can make them more fibrous and can store growth factors, contributing to the development and expansion of fibroids.
Risk Factors for Uterine Fibroids
- Age
- Reproductive Years: Fibroids are most common in women in their 30s and 40s, during the reproductive years. The risk decreases after menopause when hormone levels drop.
- Family History
- Genetic Predisposition: Having a close relative, such as a mother or sister, with fibroids increases your risk. Studies suggest that women with a family history of fibroids are about three times more likely to develop them.
- Race
- African-American Women: African-American women are more likely to develop fibroids than women of other racial groups. They also tend to develop fibroids at a younger age, experience more severe symptoms, and are more likely to have multiple or larger fibroids.
- Obesity
- Increased Body Weight: Women who are overweight or obese are at a higher risk of developing fibroids. The risk increases with the degree of obesity, likely due to higher levels of estrogen produced by fat cells.
- Diet
- Red Meat and Alcohol: A diet high in red meat (especially beef and ham) and alcohol consumption has been linked to a higher risk of fibroids. Conversely, a diet rich in green vegetables, fruit, and low-fat dairy products may lower the risk.
- Early Menstruation
- Early Onset of Menstruation: Starting menstruation at an early age (before age 10) is associated with a higher risk of developing fibroids later in life, likely due to longer exposure to estrogen and progesterone.
- Vitamin D Deficiency
- Lack of Vitamin D: Some studies suggest that women with lower levels of vitamin D are at an increased risk of developing fibroids. Vitamin D is thought to inhibit fibroid cell growth.
- Lifestyle Factors
- Lack of Physical Activity: Sedentary behavior and lack of exercise have been associated with a higher risk of fibroids. Regular physical activity may reduce the risk by helping to maintain a healthy weight and hormone levels.
- Smoking: Some studies have shown a reduced risk of fibroids in smokers, possibly due to the anti-estrogenic effect of smoking. However, smoking has numerous other harmful health effects and is not recommended as a preventive measure.
Diagnosis
The diagnosis of uterine fibroids typically involves a combination of a medical history review, physical examinations, and various imaging techniques. Here’s an overview of the diagnostic process:
1. Medical History
- Symptom Review: The healthcare provider will ask about your symptoms, including the nature and duration of menstrual bleeding, pelvic pain or pressure, urinary frequency, and any issues related to fertility or pregnancy.
- Menstrual History: Details about the menstrual cycle, such as the regularity, length, and heaviness of periods, are important in assessing the likelihood of fibroids.
- Family History: A family history of fibroids or other gynecological conditions may also be discussed, as it can influence the risk.
2. Physical Examination
- Pelvic Examination: During a pelvic exam, the healthcare provider checks for abnormalities in the shape and size of the uterus. Enlarged or irregularly shaped uterine contours may suggest the presence of fibroids.
3. Imaging Tests
Imaging is crucial for confirming the presence, size, and location of fibroids.
- Ultrasound of Uterine Fibroids
- Transabdominal Ultrasound: A probe is placed on the abdomen to create images of the uterus. This is often the first imaging test performed and can provide a general view of the uterus.
- Transvaginal Ultrasound: A probe is inserted into the vagina to get closer to the uterus, offering more detailed images, especially of smaller fibroids or those located in the uterine lining.
- Magnetic Resonance Imaging (MRI)
- Detailed Imaging: MRI provides a more detailed picture of the uterus and fibroids, showing their size, number, and exact location. It’s particularly useful for planning surgical treatment or assessing fibroids in women with multiple or large growths.
- Hysterosonography (Sonohysterography)
- Enhanced Ultrasound: This technique involves infusing saline into the uterus during an ultrasound. It provides a clearer view of the uterine cavity and is particularly useful for detecting submucosal fibroids.
- Hysterosalpingography
- X-ray Imaging: In this procedure, a dye is injected into the uterus and fallopian tubes before an X-ray is taken. It helps to identify abnormalities in the uterine cavity and assess the fallopian tubes, often used in fertility evaluations.
- Hysteroscopy
- Direct Visualization: A hysteroscope, a thin, lighted tube, is inserted through the cervix into the uterus. This allows the doctor to directly view the inside of the uterus and identify fibroids, particularly submucosal ones. It can be combined with procedures to remove fibroids during the same session.
4. Laboratory Tests
- Blood Tests: While not directly diagnosing fibroids, blood tests may be conducted to check for anemia if you’re experiencing heavy menstrual bleeding. Hormone levels might also be checked to rule out other conditions.
5. Endometrial Biopsy
- Tissue Sampling: In some cases, a small sample of the uterine lining (endometrium) may be taken to rule out other causes of abnormal bleeding, such as endometrial hyperplasia or cancer. This procedure is generally not used to diagnose fibroids but may be done as part of a broader diagnostic process.
6. Additional Diagnostic Procedures
- Laparoscopy: In certain cases, especially when other pelvic conditions are suspected, a laparoscopy may be performed. This minimally invasive surgical procedure involves inserting a camera through a small incision in the abdomen to view the outside of the uterus and other pelvic organs. It’s not commonly used for fibroid diagnosis but may be considered in complex cases.
Treatment Options
In recent years, significant advancements have been made in the treatment of uterine fibroids, focusing on less invasive methods, improved symptom management, and fertility preservation. Here are some of the latest developments:
1. Medications
- Elagolix with Add-Back Therapy: This FDA-approved oral medication works by suppressing ovarian hormone production, reducing fibroid size and related symptoms. The addition of “add-back” therapy (small doses of estrogen and progesterone) helps to mitigate the side effects of hormone suppression, such as bone loss.
- Selective Progesterone Receptor Modulators (SPRMs): Drugs like ulipristal acetate have shown promise in reducing fibroid size and controlling bleeding by modulating progesterone activity in the uterus.
2. Minimally Invasive Procedures
- Uterine Fibroid Embolization (UFE): This procedure involves blocking the blood supply to fibroids, causing them to shrink. It’s an effective alternative to surgery with a shorter recovery time and is increasingly recommended for women who wish to avoid hysterectomy.
- Magnetic Resonance-Guided Focused Ultrasound (MRgFUS): This non-invasive treatment uses high-intensity ultrasound waves to heat and destroy fibroid tissue. Guided by MRI, MRgFUS is a precise and effective option with minimal side effects.
3. Surgical Innovations
- Hysteroscopic Myomectomy: For women with submucosal fibroids, this procedure allows for the removal of fibroids through the vagina and cervix without any abdominal incisions, preserving the uterus and fertility.
- Laparoscopic and Robotic Myomectomy: These minimally invasive surgeries allow for the removal of fibroids while preserving the uterus. Robotic assistance can enhance precision, reduce recovery time, and minimize scarring.
4. Lifestyle and Dietary Interventions
- Dietary Changes: Recent studies suggest that a diet rich in fruits, vegetables, and whole grains, combined with reduced red meat and alcohol consumption, may help manage fibroid symptoms and reduce the risk of their development.
- Exercise and Weight Management: Regular physical activity and maintaining a healthy weight can reduce the severity of symptoms and the risk of developing fibroids.
5. Gene Therapy and Molecular Targeting
- Emerging Therapies: Research is ongoing into gene therapy and molecular targeting to develop treatments that can more specifically target fibroid growth factors and hormonal pathways. While still in experimental stages, these therapies hold promise for the future of fibroid treatment.
Foods To Shrink Uterine Fibroids
Certain foods may help manage or reduce the size of uterine fibroids by balancing hormones and reducing inflammation. Here are some foods that may help:
- Leafy Greens: Vegetables like spinach, kale, and broccoli are rich in antioxidants and can help reduce inflammation.
- Fruits: Berries, apples, and citrus fruits are high in fiber and antioxidants, which may help regulate hormone levels.
- Whole Grains: Foods like brown rice, quinoa, and oats can help stabilize blood sugar levels, reducing the risk of fibroid growth.
- Legumes: Beans, lentils, and peas are high in fiber and can help maintain hormone balance.
- Green Tea: Contains antioxidants, particularly epigallocatechin gallate (EGCG), which may help reduce fibroid size.
- Fatty Fish: Salmon, mackerel, and sardines are rich in omega-3 fatty acids, which have anti-inflammatory properties.
- Flaxseeds: Rich in lignans and omega-3s, flaxseeds can help balance estrogen levels.
It’s important to note that while diet can help manage fibroid symptoms, it may not be sufficient to shrink them significantly. Always consult with a healthcare provider for a comprehensive treatment plan.
Conclusion
Uterine fibroids are a common but manageable condition with a range of treatment options available, from lifestyle changes to advanced surgical techniques. The latest research continues to expand the possibilities for less invasive, more effective treatments, offering hope for women seeking relief from fibroid-related symptoms. If you suspect you have fibroids or are experiencing symptoms, consult with a healthcare provider to explore the best treatment options for your needs.
Disclaimer: This information provides a general overview of diagnosis, treatment, and medication related to alopecia areata. It is intended to assist in understanding potential options but is not comprehensive. This content is not a substitute for professional medical advice, diagnosis, or treatment. It does not cover all possible conditions, treatments, side effects, or risks specific to individual cases. For personalized medical advice, please consult a healthcare provider who can evaluate your unique circumstances. This information does not endorse or validate any specific treatments or medications.
Faqs
Can uterine fibroids cause weight gain?
Yes, uterine fibroids can cause weight gain, mainly due to the physical weight of large fibroids and abdominal swelling.
Can uterine fibroids cause infertility?
Yes, uterine fibroids can cause infertility, especially if they distort the shape of the uterus, block the fallopian tubes, or interfere with the implantation of an embryo. However, not all fibroids lead to infertility, and many women with fibroids can conceive without issues.
Can uterine fibroids burst?
While uterine fibroids generally do not burst, they can sometimes degenerate, leading to severe pain and other symptoms. A burst fibroid is extremely rare but can occur if a fibroid outgrows its blood supply, leading to a type of degeneration that might cause intense pain and bleeding. If you suspect this, it's essential to seek medical attention immediately.
Do uterine fibroids cause miscarriage?
Yes, uterine fibroids can increase the risk of miscarriage, particularly if they are large or located within the uterine cavity. Fibroids can interfere with the implantation of the embryo, restrict blood flow to the placenta, or cause structural abnormalities in the uterus, all of which can contribute to a higher risk of miscarriage. However, many women with fibroids have successful pregnancies.
Can uterine fibroids cause diarrhea?
Yes, uterine fibroids can cause diarrhea, though it is less common. Large fibroids can press against the bowels, leading to gastrointestinal symptoms such as diarrhea, constipation, or bloating. The location and size of the fibroids often determine the type of symptoms experienced.
Can uterine fibroids turn cancerous?
Uterine fibroids are almost always benign (non-cancerous). However, in very rare cases, a fibroid can develop into a type of cancer called leiomyosarcoma. The risk of this happening is extremely low, estimated at less than 1 in 1,000. Most fibroids do not increase the risk of uterine cancer.
Do uterine fibroids shrink after menopause?
Yes, uterine fibroids often shrink after menopause. This happens because estrogen and progesterone levels, which contribute to fibroid growth, decrease significantly after menopause. As a result, fibroids typically reduce in size and symptoms may improve. However, in some cases, fibroids can still cause symptoms or complications even after menopause.
Can you get pregnant with uterine fibroids?
Yes, you can get pregnant with uterine fibroids. Many women with fibroids conceive and have healthy pregnancies.
Why do uterine fibroids cause bleeding?
Uterine fibroids can cause bleeding because they can interfere with the normal structure and function of the uterus. They may: Distort the Uterine Lining: Fibroids can change the shape of the uterine cavity, leading to abnormal bleeding. Increase Blood Flow: They can cause an increase in blood flow to the uterus, resulting in heavy or prolonged menstrual bleeding. Cause Endometrial Changes: Fibroids can affect the endometrial lining, leading to irregular bleeding or spotting. These disruptions can lead to symptoms like heavy menstrual bleeding, spotting between periods, or even bleeding after menopause.
herbal tea for uterine fibroids
Herbal teas such as green tea, ginger tea, turmeric tea, raspberry leaf tea, and chaste tree (Vitex) tea may help manage symptoms of uterine fibroids.
Can uterine fibroids cause discharge?
Yes, uterine fibroids can cause discharge. Abnormal vaginal discharge can occur due to the impact of fibroids on the uterine lining, which may lead to increased bleeding or spotting that appears as discharge. If you're experiencing unusual discharge, it's a good idea to consult a healthcare provider to determine the cause and appropriate treatment.