Taking a Breath: Understanding Pneumonia
Pneumonia is a significant and potentially life-threatening infection of the lungs that affects millions of people worldwide each year. This blog provides a comprehensive overview of pneumonia, covering its types, causes, pathogenesis, clinical features, management strategies, prevention methods, and concluding remarks.
Types
Pneumonia can be classified in various ways, depending on the location and cause:
-
Anatomical Classification:
- Lobar Pneumonia: Affects an entire lobe of the lung, often caused by bacteria.
- Bronchopneumonia: Patchy inflammation in the airways and surrounding lung tissue, commonly caused by bacteria or viruses.
-
Clinical Classification:
- Community-Acquired Pneumonia (CAP): The most common type, contracted outside of a hospital setting.
- Hospital-Acquired Pneumonia (HAP): Develops during hospitalization, often involving more resistant bacteria.
- Aspiration Pneumonia: Caused by inhaling foreign material, like food or vomit, into the lungs.
-
Etiological Classification:
- Bacterial : Most commonly caused by Streptococcus pneumoniae.
- Viral : Often caused by viruses like influenza or respiratory syncytial virus (RSV).
- Fungal : Less common, caused by fungi like Aspergillus.
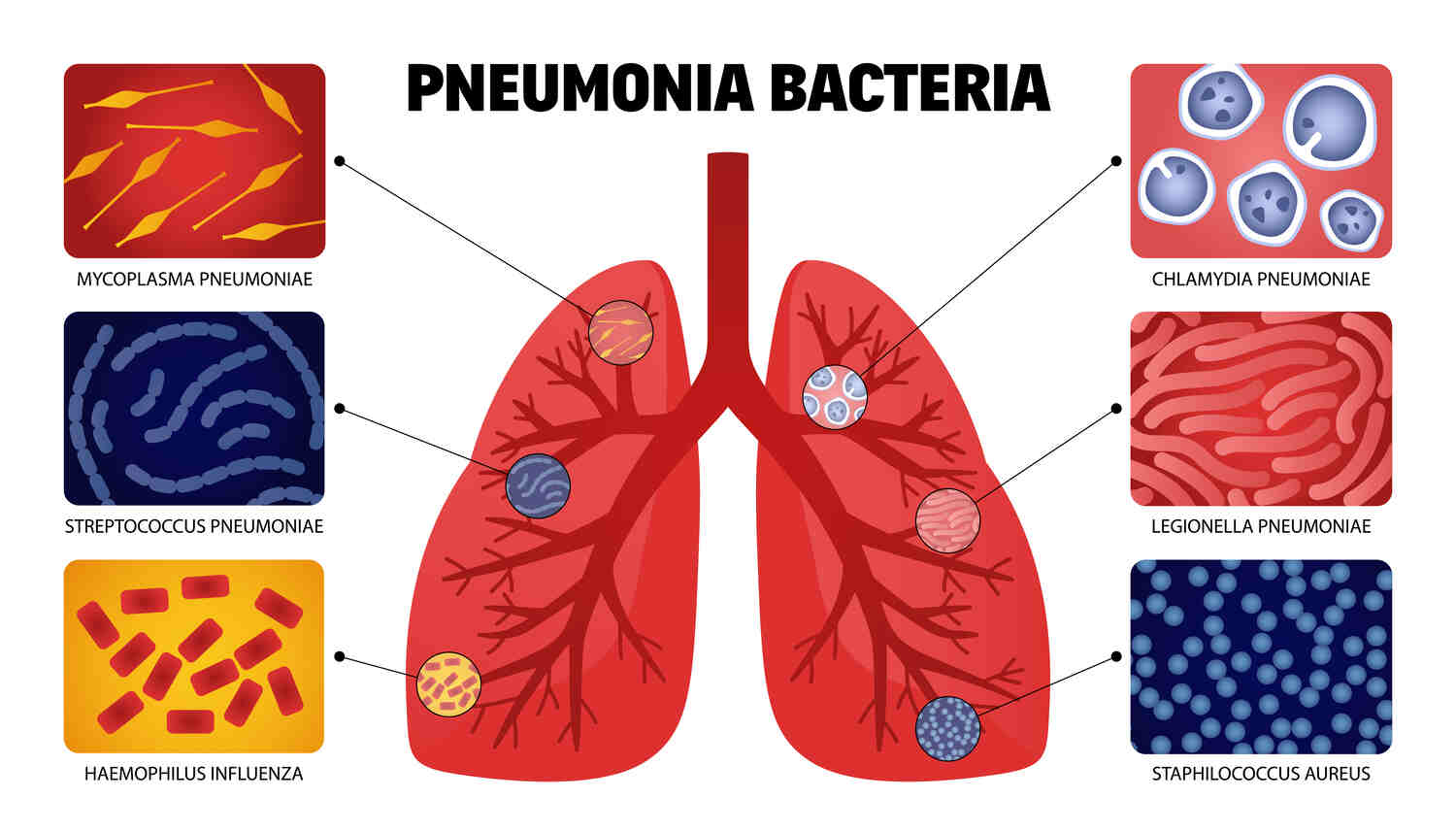
Unveiling the Culprits: Etiology
Bacterial Pneumonia
- Streptococcus pneumoniae:
- The most common cause of community-acquired pneumonia (CAP).
- Causes lobar pneumonia, characterized by consolidation of a single lobe of the lung.
- Haemophilus influenzae:
- Common in patients with underlying lung diseases such as chronic obstructive pulmonary disease (COPD).
- Can cause both CAP and hospital-acquired pneumonia (HAP).
- Staphylococcus aureus:
- Can cause severe chest infection, especially after influenza infection.
- Methicillin-resistant Staphylococcus aureus (MRSA) is a significant cause of HAP and ventilator-associated pneumonia (VAP).
- Klebsiella pneumoniae:
- Often associated with aspiration pneumonia and alcohol use disorder.
- Causes necrotizing pneumonia with “currant jelly” sputum.
- Pseudomonas aeruginosa:
- Common in patients with cystic fibrosis, bronchiectasis, and those who are immunocompromised.
- A major cause of HAP and VAP.
- Legionella pneumophila:
- Causes Legionnaires’ disease, a severe form of chest infection.
- Acquired from contaminated water sources (e.g., air conditioning systems).
- Mycoplasma pneumoniae:
- Atypical pneumonia, often in younger adults and school-aged children.
- Causes a milder form of infection known as “walking pneumonia.”
- Chlamydophila pneumoniae:
- Another cause of atypical pneumonia.
- Typically presents with a prolonged, mild respiratory illness.
Viral Pneumonia
- Influenza Virus:
- A major cause of viral pneumonia, particularly during flu season.
- Can lead to secondary bacterial pulmonary infection.
- Respiratory Syncytial Virus (RSV):
- Common in infants and young children.
- Can cause severe lower respiratory tract infections.
- Coronavirus:
- Includes viruses like SARS-CoV-2 (causing COVID-19), which can lead to severe infection and acute respiratory distress syndrome (ARDS).
- Adenovirus:
- Can cause pulmonary infection in both children and adults.
- Often associated with military recruits and closed populations.
- Human Metapneumovirus:
- Similar to RSV in its presentation and population affected (mainly children and elderly).
Fungal Pneumonia
- Histoplasma capsulatum:
- Causes histoplasmosis, often found in the Ohio and Mississippi River valleys.
- Acquired from inhaling spores from bird or bat droppings.
- Coccidioides immitis:
- Causes coccidioidomycosis (Valley fever), common in the Southwestern United States.
- Acquired from inhaling fungal spores from disturbed soil.
- Aspergillus species:
- Causes aspergillosis, often in immunocompromised patients or those with pre-existing lung conditions.
- Cryptococcus neoformans:
- Causes cryptococcosis, primarily in immunocompromised individuals (e.g., HIV/AIDS patients).
- Acquired from inhaling soil contaminated with bird droppings.
Parasitic Pneumonia
- Toxoplasma gondii:
- Causes toxoplasmosis, particularly in immunocompromised individuals.
- Acquired from undercooked meat or exposure to cat feces.
- Strongyloides stercoralis:
- Causes strongyloidiasis, which can lead to severe pulmonary infection in immunocompromised patients.
- Acquired through skin contact with contaminated soil.
- Paragonimus westermani:
- Causes paragonimiasis, also known as lung fluke disease.
- Acquired from eating undercooked or raw freshwater crabs or crayfish.
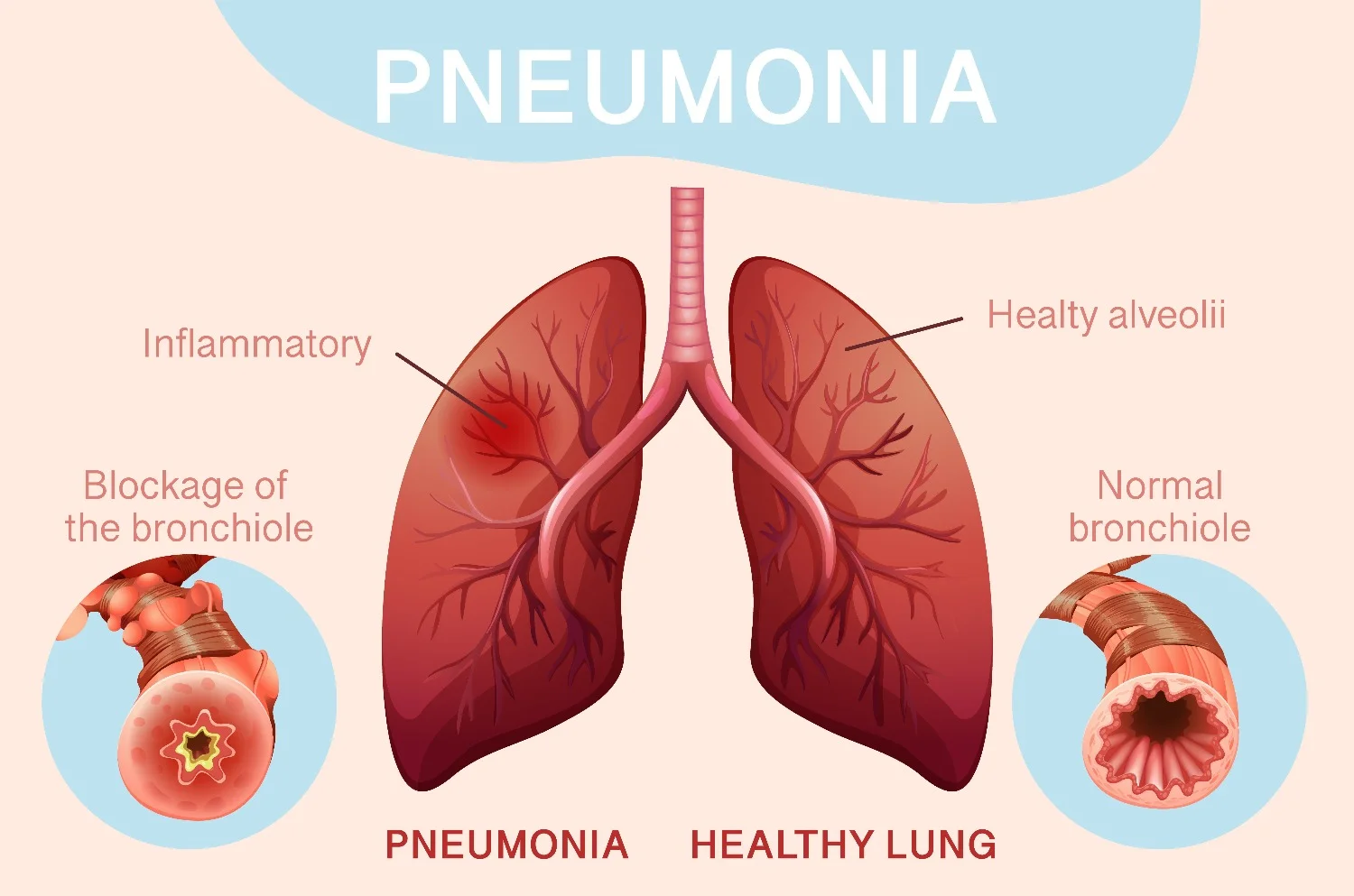
The Path of Infection: Pathogenesis
The pathogenesis of involves several key steps:
- Colonization and Invasion:
- Pathogens colonize the nasopharynx and then invade the lower respiratory tract, often following a breach in the body’s defense mechanisms (e.g., impaired cough reflex, mucociliary clearance).
- Inflammatory Response:
- The immune system responds to the infection by releasing inflammatory mediators, leading to increased blood flow and permeability in the alveolar capillaries.
- Consolidation:
- Exudates, including fluid, inflammatory cells, and cellular debris, accumulate in the alveoli, causing consolidation (solidification) of lung tissue.
- Impaired Gas Exchange:
- The accumulation of exudate in the alveoli impairs gas exchange, leading to hypoxemia (low blood oxygen levels).
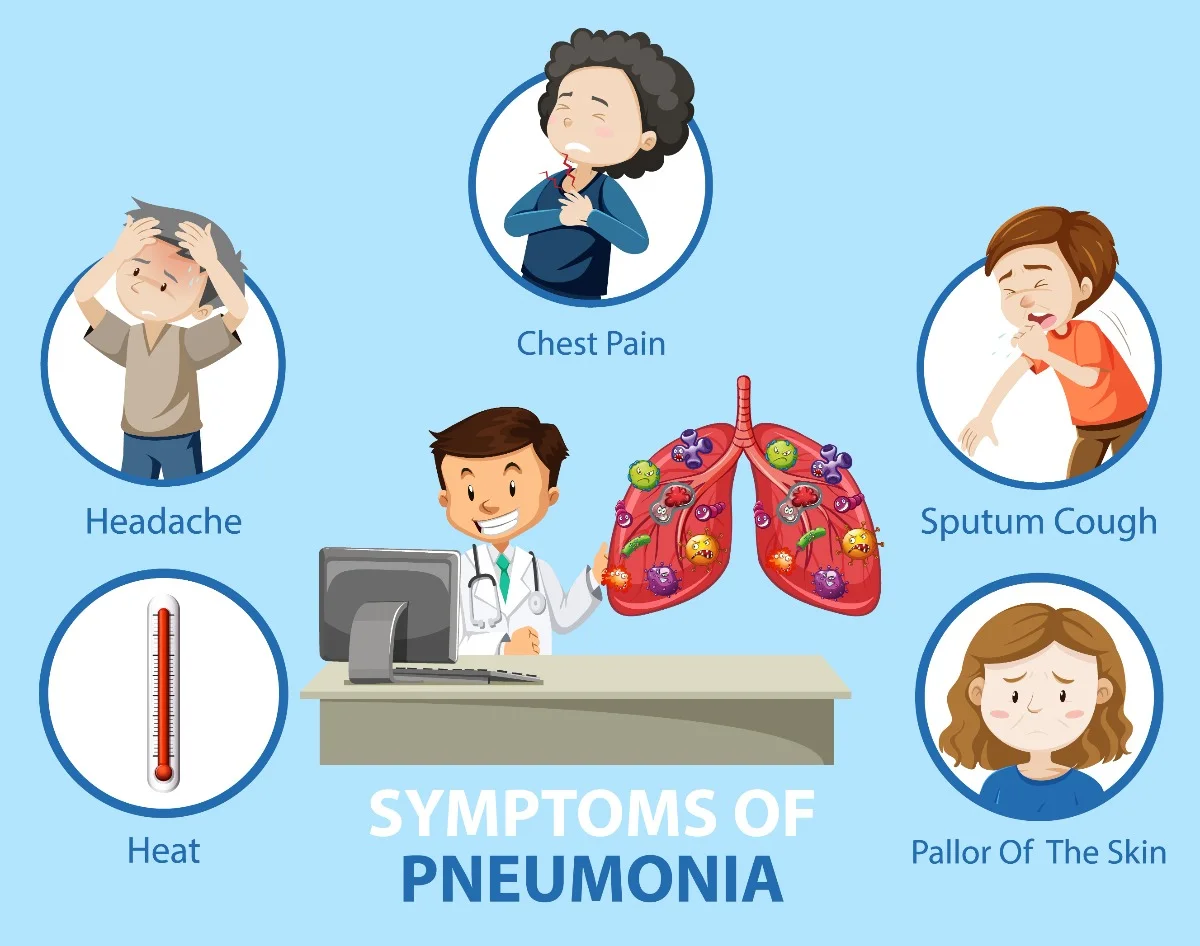
Recognizing the Signs: Clinical Features
General Symptoms
- Fever:
- High fever is common, though some elderly or immunocompromised patients might present with lower or absent fever.
- Chills:
- Shaking chills (rigors) can occur, especially with bacterial pneumonia.
- Fatigue:
- General malaise and tiredness are frequent.
- Sweating:
- Profuse sweating, particularly at night.
Respiratory Symptoms
- Cough:
- Persistent cough, which may be productive (producing sputum) or dry.
- Sputum can be clear, yellow, green, or even blood-tinged.
- Shortness of Breath:
- Dyspnea, or difficulty breathing, which can range from mild to severe.
- Increased respiratory rate (tachypnea).
- Chest Pain:
- Pleuritic chest pain that worsens with deep breathing, coughing, or sneezing.
- Often sharp or stabbing in nature.
- Wheezing:
- Wheezing can occur, particularly in patients with underlying asthma or COPD.
Physical Examination Findings
- Crackles (Rales):
- Fine or coarse crackling sounds heard on lung auscultation, often at the bases.
- Decreased Breath Sounds:
- Reduced or absent breath sounds in areas of lung consolidation.
- Bronchial Breath Sounds:
- Harsh breath sounds heard over areas of consolidation.
- Dullness to Percussion:
- Dull sound on tapping (percussion) over the affected lung area, indicating fluid or solid tissue instead of air.
- Tactile Fremitus:
- Increased vibration felt on the chest wall during speaking, over consolidated areas.
Systemic Symptoms
- Headache:
- Common, especially in viral or atypical pulmonary infection.
- Myalgia:
- Muscle pain or body aches.
- Joint Pain:
- Arthralgia, common with some viral infection.
- Nausea and Vomiting:
- Gastrointestinal symptoms can be present, especially in children.
Severe Cases
- Cyanosis:
- Bluish tint to the lips, skin, or nails due to low oxygen levels.
- Confusion or Altered Mental Status:
- Particularly in elderly patients, who may present with confusion or delirium instead of typical respiratory symptoms.
- Hypotension:
- Low blood pressure, possibly leading to septic shock.
- Hypoxemia:
- Low oxygen levels in the blood, measured by pulse oximetry or arterial blood gases.
Specific Features Based on Pathogen
- Bacterial Pneumonia:
- Often presents with sudden onset of high fever, productive cough with purulent sputum, and pleuritic chest pain.
- Streptococcus pneumoniae: Rust-colored sputum.
- Klebsiella pneumoniae: Currant jelly sputum.
- Viral Pneumonia:
- May present with a more gradual onset, accompanied by systemic symptoms like headache, myalgia, and fatigue.
- Influenza: Rapid onset with high fever, muscle aches, and dry cough.
- SARS-CoV-2 (COVID-19): Fever, cough, shortness of breath, loss of taste or smell.
- Atypical Pneumonia:
- Generally milder symptoms with a gradual onset.
- Mycoplasma pneumoniae: Often in younger adults, with dry cough, headache, and low-grade fever.
- Legionella pneumophila: High fever, diarrhea, hyponatremia (low sodium levels), and confusion.
- Aspiration Pneumonia:
- Occurs after inhalation of foreign material.
- Symptoms include cough, fever, and respiratory distress, often in patients with a history of dysphagia or altered consciousness.
Diagnosis
Diagnosing pneumonia involves a combination of clinical evaluation, imaging studies, and laboratory tests. The aim is to confirm the presence of pulmonary infection, identify the causative pathogen, and assess the severity of the disease. Here is a detailed overview of the diagnostic process :
Clinical Evaluation
- Medical History:
- Symptom assessment: Onset, duration, and characteristics of cough, fever, shortness of breath, chest pain, and other related symptoms.
- Past medical history: Previous respiratory infections, chronic diseases (e.g., COPD, diabetes), immunosuppressive conditions, smoking history.
- Recent exposures: Contact with sick individuals, travel history, occupational risks, and living conditions.
- Physical Examination:
- Vital Signs: Assess for fever, tachycardia, tachypnea, and oxygen saturation levels.
- Respiratory Examination:
- Inspection: Look for signs of respiratory distress, use of accessory muscles, and cyanosis.
- Palpation: Assess for increased tactile fremitus over consolidated areas.
- Percussion: Dullness to percussion over areas of consolidation.
- Auscultation: Listen for abnormal breath sounds such as crackles (rales), bronchial breath sounds, and decreased breath sounds.
Imaging Studies
- Chest X-ray:
- The first-line imaging modality to confirm the presence of pneumonia.
- Findings: Consolidation, interstitial infiltrates, pleural effusion, and cavitation.
- Helps differentiate between lobar, broncho and interstitial pneumonia.
- Computed Tomography (CT) Scan:
- Indicated in complicated cases or when chest X-ray findings are inconclusive.
- Provides detailed images to assess the extent of infection, identify abscesses, and detect underlying lung pathology.
Laboratory Tests
- Blood Tests:
- Complete Blood Count (CBC): Elevated white blood cell (WBC) count indicates infection; however, low WBC count can be seen in severe cases or immunocompromised patients.
- C-reactive Protein (CRP) and Erythrocyte Sedimentation Rate (ESR): Elevated levels indicate inflammation.
- Procalcitonin: Elevated levels suggest bacterial infection and help guide antibiotic therapy.
- Microbiological Tests:
- Sputum Gram Stain and Culture:
- Collection of sputum sample to identify bacterial pathogens.
- Gram stain provides preliminary information on the type of bacteria.
- Blood Cultures:
- Collected in cases of severe pulmonary infection or suspected bacteremia.
- Pleural Fluid Analysis:
- Indicated if pleural effusion is present.
- Analyzed for pathogens, cell count, and chemistry.
- Sputum Gram Stain and Culture:
- Polymerase Chain Reaction (PCR) and Antigen Detection:
- Rapid tests to detect specific viral or atypical bacterial pathogens (e.g., influenza, Mycoplasma pneumoniae, Legionella pneumophila).
- Urinary Antigen Tests:
- Useful for detecting Legionella pneumophila and Streptococcus pneumoniae antigens.
- Serology:
- Detects antibodies against atypical pathogens (e.g., Mycoplasma, Chlamydophila) but is less commonly used due to availability of faster PCR methods.
Special Diagnostic Procedures
- Bronchoscopy:
- Indicated in cases of severe pneumonia, immunocompromised patients, or when initial tests are inconclusive.
- Allows for direct visualization, bronchoalveolar lavage (BAL), and biopsy if needed.
- Thoracentesis:
- Performed if there is a significant pleural effusion.
- Fluid is analyzed for signs of infection, malignancy, or other causes.
Severity Assessment Tools
-
CURB-65 Score:
- Assesses the severity of pneumonia and helps guide the decision for hospitalization.
- Criteria: Confusion, Urea >7 mmol/L, Respiratory rate ≥30/min, Blood pressure (systolic <90 mmHg or diastolic ≤60 mmHg), Age ≥65 years.
-
Pneumonia Severity Index (PSI):
- A more comprehensive scoring system to determine the severity and risk of mortality in pneumonia patients.
Taking Charge: Management
Managing pneumonia involves a combination of antimicrobial therapy, supportive care, and specific interventions based on the severity and types. The goals of treatment are to eradicate the infection, relieve symptoms, and prevent complications. Here’s a comprehensive guide:
Antimicrobial Therapy
-
Community-Acquired Pneumonia (CAP):
- Outpatient Treatment:
- Previously Healthy Patients: Empirical therapy with a macrolide (e.g., azithromycin, clarithromycin) or doxycycline.
- Patients with Comorbidities (e.g., diabetes, heart disease): Combination therapy with a beta-lactam (e.g., amoxicillin-clavulanate) plus a macrolide or a respiratory fluoroquinolone (e.g., levofloxacin, moxifloxacin).
- Inpatient Treatment:
- Non-ICU: A beta-lactam (e.g., ceftriaxone, cefotaxime) plus a macrolide or a respiratory fluoroquinolone.
- ICU: A beta-lactam (e.g., ceftriaxone, cefotaxime) plus either azithromycin or a respiratory fluoroquinolone. Consider adding MRSA or Pseudomonas coverage if risk factors are present (e.g., vancomycin or piperacillin-tazobactam).
- Outpatient Treatment:
-
Hospital-Acquired Pneumonia (HAP) and Ventilator-Associated Pneumonia (VAP):
- Empirical broad-spectrum antibiotic therapy is often required due to the risk of multidrug-resistant organisms.
- Options include antipseudomonal beta-lactams (e.g., piperacillin-tazobactam, meropenem) plus MRSA coverage (e.g., vancomycin, linezolid).
- De-escalation based on culture results and clinical response.
-
Aspiration Pneumonia:
- Coverage for anaerobes and typical oral flora is recommended (e.g., amoxicillin-clavulanate or clindamycin).
-
Atypical Pneumonia:
- Treatment tailored to the specific pathogen:
- Mycoplasma pneumoniae and Chlamydophila pneumoniae: Macrolides, doxycycline, or fluoroquinolones.
- Legionella pneumophila: Macrolides or fluoroquinolones.
- Treatment tailored to the specific pathogen:
Supportive Care
- Oxygen Therapy:
- Supplemental oxygen to maintain adequate oxygen saturation (SpO2 > 90%).
- Non-invasive ventilation or mechanical ventilation for severe respiratory distress or failure.
- Fluid Management:
- Adequate hydration to maintain fluid balance and support organ function.
- Avoid overhydration to prevent exacerbating pulmonary edema.
- Antipyretics and Analgesics:
- Medications like acetaminophen or ibuprofen to manage fever and pain.
- Nutritional Support:
- Ensure proper nutrition to support immune function and recovery.
Hospitalization Criteria
- Severe pneumonia or high-risk patients often require hospitalization.
- Criteria for hospitalization may include:
- Respiratory rate >30 breaths per minute
- Hypoxemia (SpO2 < 90% on room air)
- Multilobar involvement on lung x ray for pneumonia
- Confusion or altered mental status
- Hemodynamic instability (e.g., low blood pressure, shock)
- Significant comorbidities
Monitoring and Follow-Up
- Regular monitoring of vital signs, oxygenation, and clinical status.
- Repeat chest imaging if there is no clinical improvement or if complications are suspected.
- Follow-up visits to ensure resolution of symptoms and complete recovery.
Prevention
- Pneumonia Vaccine Guidelines:
- Pneumococcal Vaccines: PCV13 (Prevnar 13) and PPSV23 (Pneumovax 23) for children, adults over 65, and high-risk individuals.
- Influenza Vaccine: Annual vaccination to prevent flu-related pulmonary infection.
- COVID-19 Vaccine: To reduce the risk of severe pulmonary infection from SARS-CoV-2.
- Side Effects of pneumonia vaccine: Local: Pain at injection site, redness, swelling . Systemic: Fever, fatigue, headache. muscle pain , loss of appetite, nausea.
- Hand Hygiene:
- Regular hand washing with soap and water or using hand sanitizers.
- Smoking Cessation:
- Quitting smoking to reduce lung damage and infection risk.
- Healthy Lifestyle:
- Adequate nutrition, regular exercise, and managing chronic conditions.
Conclusion
Effective management of pneumonia requires timely diagnosis, appropriate antimicrobial therapy, and comprehensive supportive care. Preventive measures, including vaccination and lifestyle modifications, play a crucial role in reducing the incidence and severity. Early recognition and prompt treatment are essential to improving outcomes and preventing complications.
Frequently Asked Questions (FAQs)
What is pneumonia?
It is an infection that inflames the air sacs (alveoli) in one or both lungs. The air sacs may fill with fluid or pus, causing cough with phlegm, fever, chills, and difficulty breathing.
What causes pneumonia?
It can be caused by a variety of pathogens, including: Bacteria: Such as Streptococcus pneumoniae, Haemophilus influenzae, Legionella pneumophila. Viruses: Including influenza, respiratory syncytial virus (RSV), and SARS-CoV-2 (COVID-19). Fungi: Like Pneumocystis jirovecii (especially in immunocompromised individuals). Other causes: Aspiration pneumonia from inhaling food, liquid, or vomit.
Who is at risk for pneumonia?
While anyone can get it, the risk is higher for: Infants and young children. Adults aged 65 and older. People with chronic medical conditions (e.g., asthma, diabetes, heart disease). Immunocompromised individuals (e.g., HIV/AIDS, cancer patients). Smokers and those with a history of lung disease.
What are the symptoms of pneumonia?
Common symptoms include: Cough (with phlegm or mucus) Fever, sweating, and chills Shortness of breath Chest pain that worsens with deep breathing or coughing Fatigue and muscle aches Nausea, vomiting, or diarrhea (less common)
How is pneumonia diagnosed?
Diagnosis typically involves: Medical history and physical examination. Chest X-ray to look for signs of lung infection. Blood tests to identify infection and inflammation. Sputum test to identify the causative pathogen. Pulse oximetry to measure blood oxygen levels.
How is pneumonia treated?
Treatment depends on the cause and severity: Bacterial: Antibiotics. Viral: Antiviral medications (if appropriate) and supportive care. Fungal: Antifungal medications. General supportive care: Rest, fluids, and over-the-counter medications to relieve symptoms like fever and pain.
Can pneumonia be prevented?
Yes, prevention strategies include: Vaccination: Pneumococcal vaccines (PCV13 and PPSV23) and annual influenza vaccine. Good hygiene: Regular hand washing and avoiding close contact with sick individuals. Healthy lifestyle: Smoking cessation, balanced diet, regular exercise, and adequate sleep. Managing chronic conditions: Proper control of underlying health issues.
What are the complications of pneumonia?
Potential complications include: Respiratory failure: Needing mechanical ventilation. Sepsis: A severe infection spreading to the bloodstream. Lung abscess: Pus formation in the lung. Pleural effusion: Fluid accumulation around the lungs.
How long does it take to recover from pneumonia?
Recovery time varies based on the individual’s age, overall health, and the severity of the pneumonia: Mild cases: A few weeks. Severe cases: Several weeks to months, with possible lingering fatigue.
When should I see a doctor for pneumonia?
Seek medical attention if you experience: Persistent high fever. Difficulty breathing or shortness of breath. Chest pain that worsens with breathing or coughing. Persistent cough, especially with discolored or bloody mucus. Confusion or changes in mental awareness (especially in older adults).
Can you get pneumonia from common cold?
While you cannot get it directly from the common cold, a cold can weaken your immune system which can lead to secondary bacterial infection. In some cases, the viruses that cause the common cold can lead to viral pneumonia.




